Of all the placental pathologies that we have encountered so far- which do you think are the most serious in terms of patient risk factors-and why? Why is this evaluation-of the placenta- often an area that gets missed or skipped over with its anomalies?
Discussion Board Week 3.............
Evaluating the placenta is very serious in reference to location. With being such a beginner I am still trying to figure out viewing the internal cervical os. If the bladder is fully distended it will be inaccurate measurements. For example > 5cm, have the pt post void. When in doubt, do EV to confirm the cervix measurement accurately. Should be 3-4 cm. (Make sure to not include the isthmus because this could compromise the length as well.)
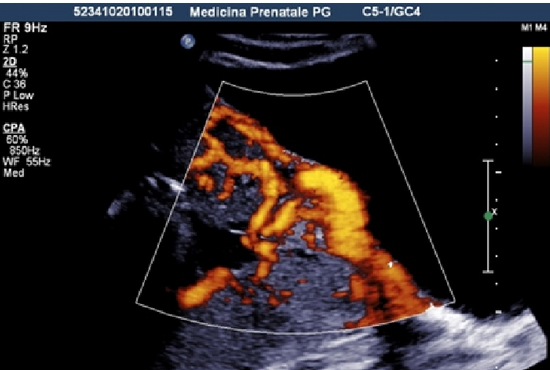
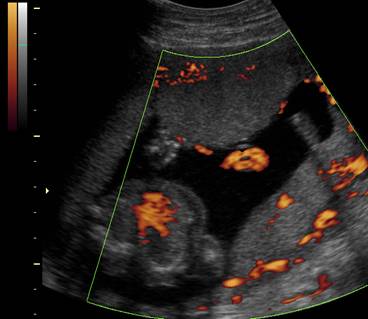
In addition differentiating Gestational Trophoblastic Disease: Chorioangioma (benign) versus choriocarcinoma (malignant). With chorioangioma displays some flow. Choriocarcinoma is super vascular. Always use color flow to help differentiate.
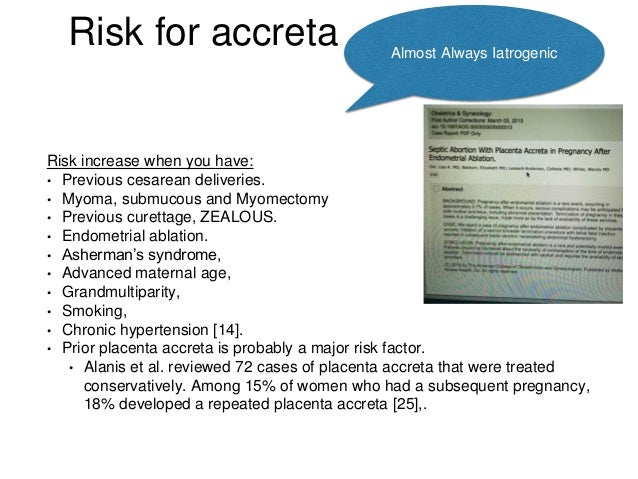
Lastly, I think Morbidly adherent placenta is serious of patient risk: Placenta increta and percreta are serious because mortality rate is high with these abnormalities. Understanding the difference "Increta" chorionic villi is deep into the myometrium, whereas "Percreta" penetrates through the myometrium and causes severe blood loss. Understanding the location of the placenta to correctly identify what type of invasion.
Thanks, Charissa! Does anyone know the sonographic visual differences between Accreta, Increta, and Percreta. How can we use echogenicity and contour to differentiate between the three?
I think we would sweep through the uterus area and uterine wall. The color flow on the placenta can allow us to visualize potential distension of tissue in the bladder or rectum. If it's distending its Placenta Percreta. For acreta, there is a break in the normal hypoechoic myometrium. I'm not sure about Increta.
Charissa, I also find it difficult sometimes to measure the cervix so I just wait till the bladder fills up. At this point I can't find another solution until my eyes will become more trained to recognizing all these variations of people's anatomy.
I observed a cervical length eval today, I found it helpful! I would recommend talking with your CI after the exam to confirm where you think the cx is located. I found this helpful. It also helps when your CI is up for questions. I agree, with the pt having a full bladder it makes everything look better, just not overly full.
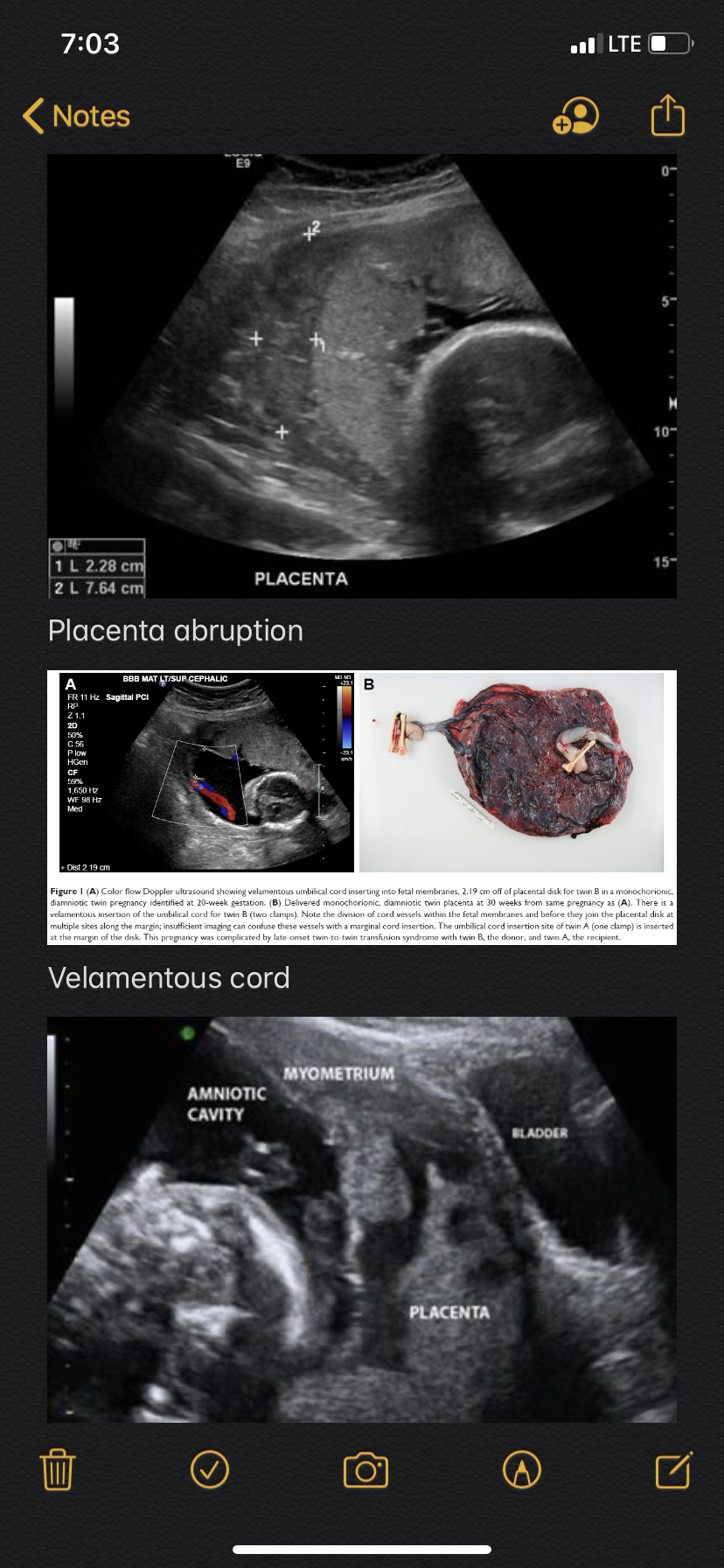
Placenta abruption is definitely one of the more serious pathologies in terms of patient risk factors due to the high mortality rate and extreme symptoms that mom may go through when this occurs.
Definition of placenta abruption: separation of a normally implanted placenta before delivery of the fetus.
Signs & symptoms (maternal): rigid/painful uterus w/ vaginal bleeding, acute renal failure, shock
Signs & symptoms (fetal): distress/demise (20-60%), IUGR, hydrops, anemia, preterm labor
I couldn’t imagine going through the pain of the placenta ripping off the uterine wall, and then having the (very high) possibility the baby dying. That must be such an emotional draining experience one has to go through, especially after carrying the little babe for so many weeks.
I think the placenta is often overlooked because we are so focused on baby’s anatomy and checking for anomalies that we forget to really assess mom’s anatomy, not just take the required images. When evaluating the placenta, we are mostly looking for location (to rule out previa) and cord insertion to make sure it is centrally located (& rule out marginal insertion). We rarely ever put color flow on the whole placenta, and after today’s lecture it makes me want to do it on every routine survey to rule out vasa previa, circumvallate placenta, placental hemorrhage, etc.
When scanning OBs, I find myself under a lot of pressure to get all of these images done in an hour (and that’s with no anomalies found). Sometimes I wish we had more than an hour for these exams. I think this is mostly because I am still a student and don’t have that scanning speed yet. Can anyone else agree?
I agree. Additionally, hearing about vas previa freaked me out a little bit. Because Michelle said that we can't see it with the naked eye due to the blood flow being anechoic. We could easily miss it! Definitely one we could miss. I like how you brought up the time crunch being a factor. Because of the rush we could easily miss something or not give an item it's due attention. I think putting color on the placenta too could help with echogenicity differentiation and grading of the placenta. Like there could be a tumor in it and we wouldn't know if the echogenicity and peripheral vascularity didn't turn us onto it. Luckily once we document the location of the placenta and the absence of any abnormal cord insertions we then just focus on grade.
Hey Amanda,
Yes placenta abruption is very scary for a fetus to encounter. When the placenta detaches itself it can cause distress on the fetus. I too think about how a mother would be feeling during this time, discomfort, vaginal bleeding and worrying about if her baby will survive. Also, adding color to R/O complications is a great idea. This can ensure that we don't miss anything with the placenta complications, or at least try our best to do everything we can, to help assess it.
I think you're absolutely right Amanda. Placental abruption is very serious and monitored very closely. We have an OB pt currently we keep evaluating. She had a questionable placenta abruption a 2-3 weeks ago. She came to us for a re-evaluation and it was a small abruption last week. We saw her again today and it's much bigger. So with this I'm assuming her care is going to change even more to best accommodate a safe pregnancy for her and her baby. As far as the time, I understand 1 hour is the standard, but I feel with pathology it will take more than an hour. Its difficult to gage that time, especially since I barely even do OB scans. It also depends at what site you go to, some places give you more than 1 hour.
Charissa, it'd be interesting to learn how this lady and her fetus will be treated. Where was the abruption? How did the sonographer document it?
Since the placenta usually grows WITH the fetus and gestational sac in size.....I'm wondering if an abruption will continue to grow. And if it does will the weight of the placenta work with gravity to pull more of the placenta away from the uterus/basalis? So with growth it's natural for the placenta abruption to get worse. And the blood will just continue to collect, take up space, and push the placenta even further away.
What do you ladies think?
This is an interesting question, Jackie. If the abruption is fairly minimal and is able to continue and be monitored, It seems to me that your hypothesis would make sense. It seems like progressively more would tear away due to gradual pulling. However, I think that most cases are not able to continue for very long before the fetus is too deprived of oxygen and nutrients (the less placenta that is attached, the less exchange) and the mother is losing too much blood. Many abruptions end quickly in preterm delivery, hysterectomy, and/or termination.
I would agree that there is more pressure being placed on technicians to get more done with less time. At my site we get 40 min for an OB and a part of my preceptors protocol is a picture of the placenta in trans and sag with and without color for reasons mentioned above. Consider yourself lucky to get 1 whole hour to complete the exam, I feel that that sort of time allows you ample time to get quality images on a moving target.
I totally agree about the time crunch. Placentas remind us how important it is to sweep! It would be so easy to take those few representative images of the placenta and move on quickly due to time, but after talking about how fatal some of these pathologies can be reminds us to sweep, sweep, sweep and really interrogate those organs so we get a full, complete story of what is going on and make sure we represent it correctly to the rad.
Thanks for sharing!
Hey All,
I had so much fun in class today learning about all the different placenta anomalies. Getting in groups really helped me understand the difference of each one better. One that has been hard for to identify is marginal, partial and complete placenta previa. I get the concept, but visualizing it on gray scale makes me nervous that I am not seeing it correctly. Nonetheless, placenta previa is a very serious issue when diagnosed with complete previa. Granted, we know the placenta normally moves away from the cervix as the pregnancy progress, however when complications arise, it can be harmful to both the fetus and the mother.
According to MedinceNet, "studies have shown a reduction in fetal growth associated with placenta previa, bleeding of placenta previa can increase the risk for preterm premature rupture of the membranes and placenta previa can have a significant emotional impact on the pregnant woman" I believe it is so important to have an eye for such previas so we can accurately document for future follow ups.
https://www.medicinenet.com/pregnancy_placenta_previa/article.htm
Here some images that I have chosen from a goggle search on placenta previa, to help train my eye. Correct me if I am wrong on these!
Complete Previa?

Low Lying?

Marginal Previa?

These are correct.
Personally, I was thinking that vasa previa is the scariest and easy to miss. Because the fetal membranes are practically invisible to our naked eye. And with vasa previa could come sucuccenturiate and velementous cord insertions. If a baby were to try to be born naturally with a vasa previa the membranes could rupture and fetal stress or demise could follow quickly.
Thanks for clarifying for me Jackie! It's pretty crazy how the placenta can grow the accessory lobe. I found that. "Sucecnturiate placenta should not be confused with placenta that covers two major aspects of the uterine cavity, which is seen frequently. In the latter condition, only a fold in the placenta separates the two parts. (This fold changes with fetal movement and with placement of the mother in a lateral decubitus position.)"
https://onlinelibrary.wiley.com/doi/pdf/10.7863/jum.1983.2.1.9
Hi Maria,
You stated that "placenta previa is a very serious issue when diagnosed with complete previa". I think this is great you recognize how important of a diagnosis this is to make. This pathology changes the course of the mother's pregnancy. Even if you're not comfortable with identifying between the two types, it is important to always measure placental tip to internal cervical os and know that a measurement of 2cm or less is suspicious and should be noted in the report.
Hi Amanda,
Thanks for the reminder. No matter what type of previa I'm having trouble with, if it is less than a 2cm gap from the internal os, I should be wary...got it! And technically as sonographers we don't need to call it, just measure right? The radiologist would be the one to call it. Also, if anyone knows this question: Is it with all Previa we don't do EV? or just partial and complete.
Thanks!
It gets missed because I'm too overwhelmed chasing a fetus around the womb to obtain my 100 or so images for the radiologist :). The placenta location typically such an easy task to check off the list. Location, distance from cervix, cord insertion and DONE. From the reading a common cause of placenta bleeding that end in fetal demise about 50% of the time are placental hematomas. These will be bleeds behind the placenta caused by the frondosum detaching. If the area of detachment is too large this will have a negative impact on the developing fetus getting all of the oxygen and nutrients it needs to progress. This does not always cause vaginal bleeding since the bleed can be contained behind the placenta so the mother may not have many symptoms for us to key in on. This is also a super common occurance which makes them something we need to take seriously. The risk for fetal demise increases with the size of the bleed. A differential would include a subchorionic hemorrhage which is the most common cause of first trimester bleeding, often associated with normal implantation.

I saw 2 subchorionic bleeds today in emergency.
How do you tell the difference between a retroplacental hemorrhage and a subchorionic hemorrhage?
I believe a subchorionic hemorrhage would be near the surface of the chorion just under the chorion/amnion fusion and a retroplacental hemorrhage would be between the placenta/uterus surface. Or maybe I have that wrong. I haven't noticed one in real time before.
We did have a patient today with increased vascularity of the placental bed today that made us question accreta, but the rad said since its the mothers first pregnancy it's highly unlikely.
Hello Heather,
I am the same way in the sense. I usually get 5mins hands on for OB survey, so I try and go for the hard things like heart views, kidneys, and tibia/fibula. I literally bypass the placenta thinking its "easy." Now, since we have started evaluating pathology I have a working knowledge of how important the size, location, and texture of the placenta is. With subchorionic hemorrhage being the most common in first trimester, during our 20 week survey we can follow-up and access the placenta for any other abnormalities. I think also being new to sonography we are really focused on catching pathology the baby may, have not realizing the pathology or IUGR could have came from something like placenta insufficiency. We just have to remember to check and access everywhere. Because like we learned from last week theca lutein cyst cause by a molar pregnancy could be in the adnexa region.
There are some serious pathologies that involve the placenta. I think that the most dangerous pathologies are placenta acreta, velamentous insertion, and placenta abruption. Placenta accreta, increta, and percreta are dangerous because the chorionic villi start attaching to the myometrium or in severe cases penetrate the uterus into the bladder. This is bad because after delivery because the mother can bleed out. According to American pregnancy association about 75% of all cases end up being placenta accreta which is less severe. The next placental pathology is a velamentous insertion of the placenta because the cord is not covered in Wharton’s jelly. Another important pathology is placenta abruption because the placenta can detach before the baby is born causing a demise due to lack of oxygen and nutrients.
Placenta Accreta: Symptoms, Risks and Treatment. (2019, October 10). Retrieved from https://americanpregnancy.org/pregnancy-complications/placenta-accreta/.
We had a patient this week that made us question placenta accreta because it was hyper vascular near the uterus. I did a little digging and if the accreta is severe (percreta) the mom will most likely have a hysterectomy. Without removing the uterus she would continue to bleed out after birth. It is a very serious condition and one of the highest causes of maternal death. Below is a list of risk factors for placenta accreta.
The placental pathology that stood out to me the most is the placental abruption - the concealed type. Placental abruption is a premature separation of the implanted placenta before delivery of the fetus. Our textbook states that mortality rate is 20-60% in these cases and placental abruption account for 15-25% of perinatal deaths. The mother may present with problems like vaginal bleeding, pain, preterm labor and a “board-like” abdominal tone. Causes are many, including history of abrupitons, short umbilical cord, placenta previa, tobacco & cocaine use, pre-eclampsia, thrombophilia. In 50% of abruptions resulting in fetal death, mothers experience hypertension.
A concealed abruption is one that doesn’t present with obvious symptoms of bleeding, but is silent and bleeds between the placenta and uterus. This results from the rupture of spiral arteries. Sonography is not very sensitive in showing this because the hemorrhage may look isoechoic to the placenta, may be smaller or may appear as thickening of placenta.
Placental abruptions are treated with an induced labor or a caesarean or if the abruption is only a small part of the placenta then the patient may be monitored closely.
I think placental pathologies are often missed because it is not given enough time, it appears as an easy evaluation and if the rest of the fetal anatomy looks ok the sonographer may not be alarmed to look closer. As a student, I think it is because there are so many pictures we need to take that we just rush through to obtain them and then sweep more slowly to check for pathology. Today I completed a limited growth on a 3rd trimester, but the only picture I couldn’t get was the placenta! It appeared sooo different from what I was “used” to seeing. It had so many calcifications and uneven curvy contour that completely distorted the whole shape and echogenicity of the placenta. I”m glad I was exposed to this placental presentation:)

Hi Elona, I agree with you that placenta abruption is very dangerous for both the mother and fetus. I think it is going to be difficult to see the blood that is trapped behind the placenta, but it will have a different echogenicity compared to the placenta to help us capture it. Also, I agree that we should evaluate the placenta more carefully for these pathologies.
Hello Elona, awesome job on completing that 3rd trimester limited growth! As for the placenta I remember from the videos there is grades of placenta throughout the pregnancy therefore its going to different stages thorough pregnancy's when the placenta will differ in appearance. And its normal however we should keep our placenta pathologies in mind as well as correlating the placenta grades.
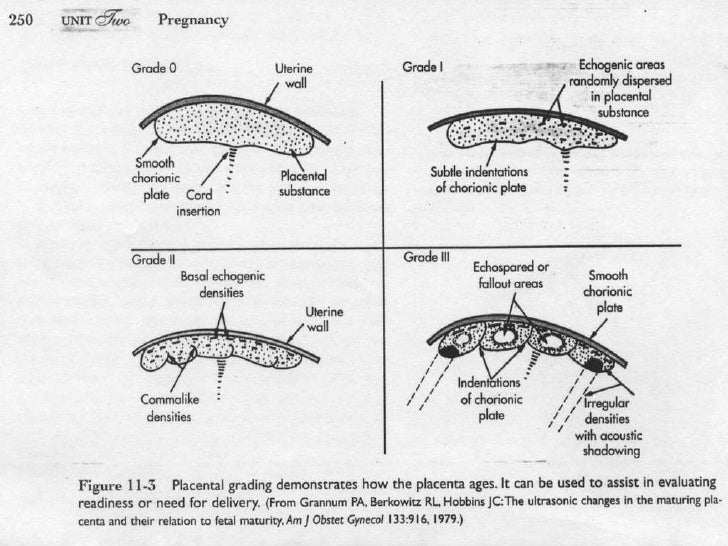 close to delivery date placenta should be presenting calcification.
close to delivery date placenta should be presenting calcification.
Elona,
this is really great information. I went through something very similar during my pregnancy where I kept having bleeds. We couldn't find the source of the bleed on ultrasound which was so confusing to me at the time. But what the Doctor shared with me is exactly this information that you shared here.
Abruptions are not always visible on ultrasound. This is one of those reasons why it is so important to take into account patient history and clinical symptoms.
In my case, it was difficult to determine whether or not is was a subchorionic hemorrhage that didn't resolve or if it was a small, chronic abruption, but we just continued to monitor it throughout pregnancy.
I think it is also important to note that unresolved hemorrhages can lead to abruption because as the blood ages, depending on size, it can cause the placenta to tear away from the wall of the uterus.
Small abruptions are easy to miss not just because of the comparable echogenicity like you mentioned, but also because if just the corner of the placenta is starting to rip away, but fluid and baby are growing just fine, the size of the amniotic sac can push the placenta in place so i appears to be attached, but when changes in position occur it can allow for the release of the blood.
Continued monitoring via ultrasound for growth parameters and fetal activity is a great way to manage these conditions.
Thank you for sharing!
Source:
Sauerbrei, E. E., & Pham, D. H. (1986). Placental abruption and subchorionic hemorrhage in the first half of pregnancy: US appearance and clinical outcome. Radiology, 160(1), 109–112. doi: 10.1148/radiology.160.1.3520643
I feel that the highest risk placental abnormalities are percreta, placenta previa, vasa previa, and retroplacental abruption.
Percreta: A placenta that has invaded beyond the uterus and into the bladder carries a high risk of premature delivery, which can be dangerous for baby. There is also high likelihood of maternal hemorrhage before, during, or after labor and often must either have a hysterectomy or methotrexate therapy to stop the hemorrhage.
Complete Previa: The thinning and spreading of the placenta to accommodate for an impending birth can separate the placenta and cause maternal hemorrhage, shock, possible c-section/hysterectomy. The baby could suffer complications from loss of oxygen, face premature delivery, and lose blood.
Vasa Previa: Due to the velamentous cord insertion and contact with the cervix, the dangers to the fetus are hemorrhage, exsanguination, or death.
Retroplacental Abruption: Due to the fact that the placenta breaks away from the uterus, it can lead to maternal hemorrhage & shock, need for blood transfusion, failure of kidneys or other organs resulting from significant blood loss, and even hysterectomy to stop bleeding. The baby can face restricted growth from not getting enough nutrients, loss of oxygen, premature birth, or even being stillborn.
Some of these abnormalities can be challenging to diagnose due to visualization issues, not thoroughly imaging the placenta in its entirety, or rushing through maternal anatomy in order to examine fetal structures. Additionally, several types of bleeding can be isoechoic to the placenta itself.
Hello Beth,
I also feel placenta percreta, placenta previa, vasa previa, and retroplacental abruption have some high risk factors in pregnancy. During your presentation one of the anomaly that you went over was circumvallate placenta. It is also a placenta anomaly and this is very important to note. We often have to travel the placenta tip to the cervix to show that it is not low- lying. With the circumvallate placenta the placenta starts to fold back on its self creating a lift in the amnion and chorion ( this can occur on the tip or center of placental surface). This can be dangerous and cause bleeding due to the fetal membranes and placental membranes being exposed. In addition, the fetus can lose blood and nutrients. This anomaly usually presents itself at 20weeks so when we do our surveys we should check the borders mothers typically do not have signs and symptoms for circumvallate placenta. It is important for us to check for any lifting, or as you stated any further growth into the myometrium placenta percreta.
https://www.healthline.com/health/pregnancy/circumvallate-placenta
How Circumvallate Placenta can effect the baby:
- IUGR
- Placenta abruption
- Oligohydramnios
- Miscarriage
- Preterm


I agree, Jazmin - circumvallate is also very dangerous. Since we have been studying placenta and umbilical cord, I have been even more careful when examining both. I have been taking much longer to look at the placenta in all dimensions and planes, making sure it is completely attached, with no bleeds, and that there are no UC vessels over the cervix!
Hello friends,
To me the most serious of all the pathologies in the placenta is a vasa previa. I've seen some if my preceptors put color on the cervix and on the placenta for the cord insertion, however, without putting the color just in front of the cervix, vasa previa can be easily missed. It can especially be missed because even though it can be seen with velamentous cord insertion, it's not always. With a normal cervix and a normal cord insertion, there may not be any clear red flags.
Without finding this, the patient's doctor wouldn't be able to direct the her with the safest practices for her situation (bed rest for instance). Without knowing this, the cervix could open to prepare for the baby's birth and the fetal membranes overlying the cervix could rupture. Depending on how far mom is from the nearest hospital, she could bleed out and there could be serious consequences for her and the baby.
To prevent something like this from happening, I think the best idea is to put a color box on the image from internal cervical os to the placental tip. This shows that there are no fetal membranes that are going to cause problems down the line.
It my opinion, it's so easy to overlook the placenta (and it's importance) because there are really one three images that we get of it (at least at my site). We get Placenta Long, Trans, and Placental CI. We don't spend too much time focusing on it, so it's easy to forget all the things that could go wrong. And if you think about it, if there is something wrong with the placenta, the chances of there being something wrong with the baby or mom is pretty high.
From now on I'm really going to take a bit more time to appreciate and thoroughly check out that placenta!
Hi Paris. What is the protocol for when to do EV and when not to do EV?
One of my techs said that less than 14 weeks is okay to do EV. Then after 14wks only EV with indications like hemorrhage, ovary issues, or excess bleeding.
Hey Jackie,
I'm not sure what the official rule is because we don't get many first trimester OB's at my site. However, it makes sense to not do it after 14 weeks because by that time mom is in her second trimester. During the 20 week anatomy scan we don't do EV unless necessary. Also, as we discussed in class, translabial seems like the safer way to go in that case.
I hope this clears things up for you.
Hi Paris,
I'm glad you get to see what we're learning in class correlate with what you observe/scan in clinicals. Vasa previa is no joke. Today I started a 2nd trimester OB survey and instantly began with the cervix. When I put the color flow on, I made sure the box was not only big enough for the cervix, but for the surrounding fluid past the internal os. I didn't see vasa previa, but caught a little bit of the floating cord at the far end of the color box. If my box was smaller and only fit the cervix itself, I can see how this important pathology could be easily missed, causing a traumatic experience for mom and baby.
Hey Amanda,
I was scanning an OB today and I had a thought. I was practicing putting color in front of the cervical canal and the baby's head was so far down. I began wondering if it was possible that I was missing a vasa previa.

In this image the baby's head is very low, but you are still able to see the vessels that are running across the internal os. I wonder if this would still be seen transabdominally. Eeepp!! Do you think we could possibly miss it if the head is super low??
To help with recognizing placenta pathology.
Can everyone post ultrasound images of different placenta pathology? And then write the answer to what it is backwards below the images, so we see the images first before the answer?
For example:
Answer: noitresni suotnemelev
I think the succenturiate placenta is the most serious in terms of patient risk factors. It develops as a result of non-involution of the chorionic leave that supposed to become smooth as soon as chorionic frondosum will attach to the decidua basalis to form a primitive placenta. As a result, usually one or sometimes more small accessory lobes of different sizes are developed in the membranes at a distance from the periphery of the main placental mass. The succenturiate lobes connected to the main placental mass via vessels of fetal origin. Because it is a rare placental anomaly (3% - 8%), it might be overlooked by a sonographer thinking that it is intrauterine contractions, a fold in the placenta, and some fibroids. Umbilical cord insertion with this type of placenta most commonly is seen into the main lobe. However, not recognizing the succenturiate placenta and determining locations of all lobes can lead to serious outcomes and complications, such as increased risk of placental infarction, placenta previa, vasa previa, heavy postpartum hemorrhage associated with retained product of conception and perinatal mortality. For instance,
- When the accessory lobe is implanted over the internal cervical os, it should be considered as a placenta previa. If underdiagnosed, cervical dilation during delivery will result in profuse hemorrhage and perinatal mortality rate can be as high as 100% because hemorrhaging can lead to fetal anemia and shock.
- Retention of the accessory lobe(s) after expulsion of the main placental mass will definitely result in serious hemorrhage.
- Hemorrhage may occur from the vessels within the membrane, which connect the succenturiate lobe to the main placental mass, because they are not protected by Warton’s jelly.
- If vascular connections between the main placental lobe and an accessory lobe go over the cervix, vasa previa is diagnosed.

Hi Ellen, it was very informative to know that a succenturiate placenta isn’t just an accessory lobe, but its a lobe that can cause problems especially if it’s located near the cervix. I did not know that if the lobe was on or near the cervix we would call the whole placenta to be previa. To know if it is part of the placenta should we be seeing flow?
Hi Lauren,
We do not like any part of the placenta to be over the cervix or within 1 cm from it. It does not matter if it is one piece placenta or an accessory lobe of the succenturiate placenta because when the cervix dilates during labor and delivery any kind of placenta previa can cause severe hemorrhage and other adverse outcomes. Therefore, it is advantageous for obstetricians to know the location or locations (if several) of accessory lobes, so they can choose appropriate delivery management plan.
Regarding your second question, with the succenturiate placenta we mostly concern with the flow in the vessels that connect main part of the placenta with the accessory lobe. Therefore, it is important to use color Doppler to find where these vessels are, especially in relation to the cervix. If vessels go over cervix, this condition must be managed as vasa previa with close follow ups.
I never thought of it this way, Ellen. You make great points about the various dangers that the accessory lobe poses. Covering the cervix and being retained post delivery put the mother and fetus at great risk of hemorrhage. Additionally, the fact that the vessels are not protected by Warton's jelly also makes the cord vulnerable to hemorrhage.
In this image, the main part of the placenta is anterior & the succenturiate lobe (*) is posterior. This type of placenta is more difficult to see, especially as the pregnancy progresses. (https://sonoworld.com/Fetus/page.aspx?id=181)

Additionally, a myometrial contraction (M) should not be confused with a succenturiate lobe of the placenta (P) or a myoma. (https://obgynkey.com/artifacts-pitfalls-and-normal-variants/)

Hi Beth,
Thank you for your great images. We really must be careful to call the placenta succenturiate. Leimyomas, folds of the placenta, and intrauterine contractions can look like an accessory lobe of the succenturiate placenta. To differentiate an intrauterine contraction from an accessory lobe, it is a good idea to rescan the doubtful region in 20 minutes. If the bulge is gone, it is most likely an intrauterine contraction. If we can find vessels connecting the main placenta with an accessory lobe by using color Doppler, it is the succenturiate placenta. Fibroids might have feeding vessels, they are located in myometrium and do not look like a part of the placenta.
Amanda mentioned that she just saw this at her site! while I do agree that this is something crazy to see I don’t think it’s necessarily always bad for the mom. For instance if the two parts of the placenta are in the fundus of the uterus than the vessels between the two may not interfere. I think this becomes dangerous when the fetal vessels cover the internal os of the cervix.
Hello Sonosistas,
You all did a great job with the most dangerous placenta anomaly that could happen I was going to pick placenta abruption, but seems you all have that one down. Another placenta anomaly we will encounter is placentomegaly and small placenta the normal placenta should be around 5cm, so once we do our initial scan we should use our subjective assessment and check location and placenta size. Having a placenta that is too large can cause fetal hydrops, maternal anemia, gestational trophoblastic disease these were from our recent quiz. Having a placenta too small can lead to placental insufficiency and IUGR. Overall having small placenta or placentomegaly will less likely lead to fetal demise. Here is an image of placentomegaly
Having placenta percreta is another serious condition of the placenta that can arise. It happens as a final stage. The placenta accreta is the first to arise only to the myometrium. Then second stage the placenta increta the placenta grows into the myometrium. Then it goes into the final stage placenta percreta where the placenta grows outside the uterus possibly as far as the bladder I remember someone asking for an ultrasound image in class so I have posted one for those visual learners. Placenta percreta is rare, but it can happen. With placenta percreta being the most severe and life -threatening for mother and baby we need to assess the borders of the placenta as well.
https://www.marchofdimes.org/complications/placental-accreta-increta-and-percreta.aspx
Hi Jazmin,
I could not agree more that the size of the placenta matters. If it is too big (> 5 cm) or too small (<2 cm), it is not good. They will lead to negative outcomes for the fetus. In addition, abnormal shape and configuration of the placenta can play a negative role in fetal growth and development. For example, the placenta membranacea is a very rare condition when chorionic frondosum failed to differentiate from chorionic laeva. As a result, placental villi cover all or almost all of the surface of the gestational membranes. Sonographically, we see much thinner placenta than normal one with placental tissue covering most of the uterine cavity. This type of placenta usually associated this antepartum and postpartum hemorrhage.

Hello!
I think all placenta abnormalities are to be taken seriously and follow up to ensure fetal well being as well as moms and ensure a safe delivery. However I believe vasa previa would be most of concern.
what is vasa previa ? vasa previa is rare, its when the fetal vessels within the run across or close the cervical os. why might you say this is of concern ? its due to the fact that these vessels are bound to rupture and cause a life threatening hemorrhage. Per our Hagen Ansert book there is two reasons that may cause vasa previa
- due to the velamentous insertion of the umbilical cord to the placental membranes which cross over the cervix
- when a succenturiate lobe is present and the connecting vessels transverse the cervix
Dr.Wilson had a great drawn picture illustrating the vessels near the cervix, this image is the closest I could find to hers
 as you can see the fetal vessels so very closely placed near the cervix is not good and concerning !
as you can see the fetal vessels so very closely placed near the cervix is not good and concerning !
Great job clarifying the causes of vasa previa ( velamentous insertion and succenturiate lobe)
I had more OB's than usual this week, many were limited follow ups, so I was able to take more time to practice evaluating the placenta as well. We had one yesterday checking for placenta previa too. I practiced using color doppler to check the internal os for vascular connections. No abnormal color flow this week thankfully, although the mom still had marginal previa even when we imaged with EV.
Below is an image of what a vasa previa due to a succenturiate lobe may look like.

Evaluating the placenta is just as important as evaluating the baby because without the placenta there is no baby to evaluate. The placenta is the conduit by which the baby receives its nutrition and oxygen so it makes sense that we need to take time and care in evaluating it. I feel like we can get so wrapped up in baby and his/her growth development that the placenta and its health get neglected.
In my opinion the placental abruption is the most serious of the conditions. It carries a fetal mortality rate of 20-60% which twice that of previa. Placental abruption is the premature separation of the placenta from the uterus. Maternal signs and symptoms can include pain, vaginal bleeding, acute renal failure, shock, and preterm labor. Fetal symptoms include IUGR which can lead to hydrops, anemia, and even death.
I think this is the most serious because it is a condition that happens suddenly and without warning. There are risk factors that make it more likely to happen such as hypertension, drug use, and trauma, however, it can also occur spontaneously. I think that along with the spontaneity and pain, the fact that the baby could be born prematurely and or die makes it the most serious. Unlike the previa (which is another serious placental problem) it is not detected on the ultrasound months in advance where one can prepare accordingly for the birth. I think also about the mental health of these women who are late in their pregnancy and have a sever abruption that leads to fetal demise because of a prolonged period of oxygen deprivation.
I completely agree with you here, Perresha. It can occur suddenly and then progress rapidly. With sometimes very little warning, the fetus and mother could completely be in jeopardy! Abruption has the potential to lead to so many very dangerous outcomes - there is decreased surface area for crucial nutrient exchange and the bleeding can be extremely severe, requiring hysterectomy to stop the bleeding, or even maternal death.
The pathology that stood out to me the most was placental abruption, when the placenta prematurely detaches from the uterine wall depriving the fetus of its blood (oxygen/nutrient) supply. The larger the the abruption is the greater the likelihood of fetal demise. This can also cause maternal blood loss and stimulate premature contractions. When a moderate-severe abruption is detected the baby needs to be delivered right away typically by c-section. A previous placental abruption increases the risk for future pregnancies (19-20%) which is why it is important to get the patient’s clinical hx pertaining to previous pregnancies before starting an exam. The placenta gets somewhat skipped over because some anomalies are hard to see with ultrasound and because we have so many other standard images pertaining directly to the fetus during routine ultrasound examinations that it gets taken for granted.
Source: https://www.marchofdimes.org/complications/placental-abruption.aspx
Source: https://radiopaedia.org/articles/placental-abruption?lang=us
Hi Serina,
I am glad that you mention that the pregnant woman can get premature contraction with placenta abruption. Hemorrhage and cramping pain are early signs and symptoms of this condition, even though they are not really specific. If we see a big placenta abruption by ultrasound, we need to report it immediately to a radiologist to prevent fetal demise if possible. I agree with you that due to the very limited time allocated to the routine second trimester fetal detail ultrasound screening placenta evaluation is often very quick and subjective. We mostly rely on our eyes, knowledge and experience to detect placental abnormalities than on actual measurements and placenta grading.
Hi, Everybody.
To wrap up this week's discussion on placenta I've attached pictures and a link to the chart I made for placental pathology. Go to the link for a larger view: https://docs.google.com/document/d/1VIymKHHTiloJCAalSi7kOqJ2IpYhvK6K6riMaQl2GZA/edit?usp=sharing
It's a lot, so I figured I'd just put it all together with the images instead of writing it all in the DB.
From our discussions it seems like the easiest thing we can do to avoid missing placenta pathology would be to put color on the placenta and the surrounding area. If we were to miss pathology it would be because we are not taking the time to appropriately assess echogenicity and surrounding structures. Just this past week I saw an emergency OB, 12 weeks. She had been to emergency 4 times. On the 2nd time the sonographer had written down perigestational hemorrhage. On the 3rd exam the sonographer had written negative for abnormality. I witnessed the 4th exam and it was obvious there was a large perigestational or subchorionic hemorrhage. OBVIOUS. However, when we were talking to the patient she said that the last sonographer had been grumpy and didn't spend too much time with her or even let her see the screen. It was apparent to us that the third sonographer had missed the hemorrhage even though it had grown in size from the 2nd exam. Perhaps the other sonographer really didn't see it. But it makes me wonder if he even checked the priors.
This story is just an example of how much influence we have over patient and pregnancy outcome. And a lot of factors can go into whether an abnormality is missed or not. The quality of the transducer, the type of exam, bladder fullness, patient's gas, patient's health, sonographer's attention, equipment available, fetus postition...all of these factors play a role in finding evidence of pathology.
Of all the placental pathologies discussed thus far I think the two most severe in terms of patient risk factors are abruption and percreta.
I am choosing to focus on percreta though as I feel it is definitely the most severe. Placental percreta is a condition in which the placenta invades the uterine wall. In placenta percreta, the vascular processes of the chorion, a fetal membrane that enters into the formation of the placenta, can invade the full thickness of the myometrium. This can cause an incomplete rupture of the uterus. The chorionic villi can go right on through both the myometrium and the outside covering of the uterus, causing complete and catastrophic rupture of the uterus. From there it can start to invade other organs and cause a complete and catastrophic mess. In fact, mortality rate is correlated to the extent of involvement of surrounding structures, which could potentially include the bladder and rectum.
When placenta percreta is complicated by bladder invasion, mortality rates have been estimated as high as 9.5% and 24% for mother and child, respectively. Knowledge of this condition and expectant management are especially important, as the incidence is on the rise—an estimated 50-fold increase in the last 50 years—attributed to the increased frequency of Caesarean deliveries. That is crazy, y'all! So keep those eyes peeled.
To get a better idea of how severe the problems can be when dealing with percreta I found a case study of of a 38-year-old woman who presented at 24 weeks gestation with vaginal bleeding and was found to have complete placenta previa with placenta percreta invading the urinary bladder. Her hospital course was complicated by bilateral pulmonary emboli. She underwent an exploratory laparotomy, repeat Caesarean section, and total abdominal hysterectomy. Because of placental invasion into the bladder, the procedure was complicated by bladder and ureter damage for which urology carried out repair.
In this case, it is amazing that the mother survived, but also a great example of how previa and percreta can often coexist and allow for invasion into the bladder. I have included and image from the case study.

Source:
Smith, Z. L., Sehgal, S. S., Arsdalen, K. N. V., & Goldstein, I. S. (2014). Placenta Percreta With Invasion into the Urinary Bladder. Urology Case Reports, 2(1), 31–32. doi: 10.1016/j.eucr.2013.11.010