Show a normal piece of fetal skeletal anatomy on an ultrasound image. State what it is and how you know it’s normal. Then, in the same post, add another image of the same piece of anatomy that is abnormal. Discuss what the anomaly is called, how you know it’s abnormal, and what may have caused this anomaly. (every student should be able to post a different anomaly on a different part of the skeleton.)
Week 9: Forum/Discussion Board
Hello Everyone,
I am so excited to be this week's moderator and see what information you each bring to share with one another! We all know how important it is to have a clear foundation of normal anatomy so when something seems askew we may document it properly even if we're not exactly sure what the condition is! As we know there are multiple classifications of skeletal dysplasias so everyone should pick something different to discuss! I look forward to doing a deeper dive with all of you into your individual anomalies and locking in this important concept!
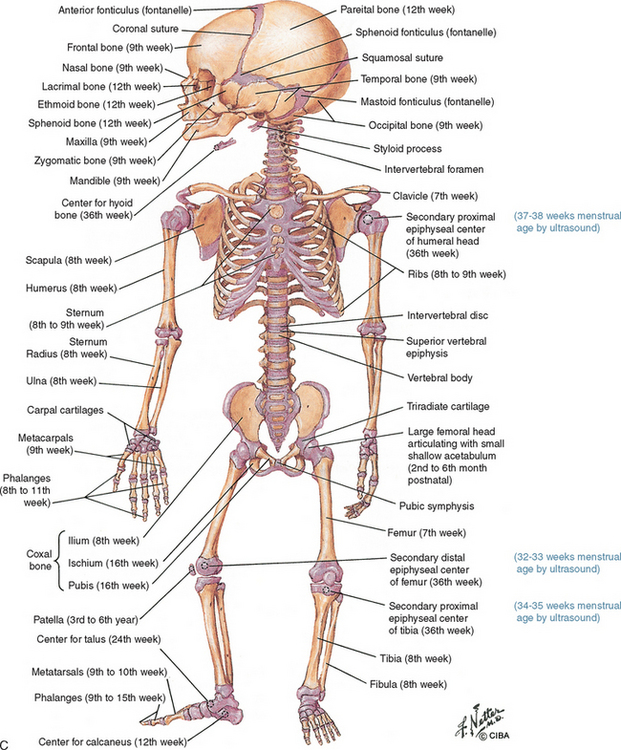
Thanks Chrishawna for starting off this week with a great, detailed diagram of the fetal skeleton with the gestational age!! So cool.
Chrishawna this picture is amazing! It is definitely the refresher I needed. I love how it includes time of development. This is great! I find it so interesting that there are bones that still developing up until at least 36 weeks.
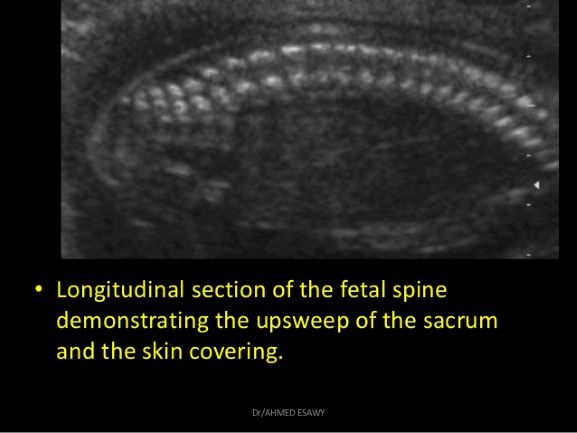
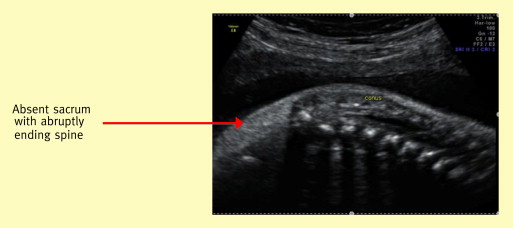
The first image below with the yellow caption underneath shows a normal fetal sacrum. The sacrum is seen at the left of the image and it has an upward sweeping motion. It is echogenic and symmetrical. The shape of the sacrum and the upward angle seen are very important signs that the sacrum is normal. The sacrum should also appear to taper at the end.
The image with the red arrow shows an abnormal sacrum. This fetus is missing a sacrum which is referred to as sacral agenesis or caudal regression syndrome. This can be determined because the caudal end of the spine does not have the typical symmetrical appearance, upward sweeping shape, and tapering at the end. The vertebrae appear to stop abruptly because there is no sacrum. This condition is rare and is seen more often when the mother is diabetic. It also is associated with a condition known as Currarino syndrome. This is a congenital condition where the fetus has anomalies in the sacral region (in the bones and soft tissues) and in the anorectum region. (https://radiopaedia.org/articles/currarino-syndrome-1?lang=us)
Hi Brittany!
Great images!
It just made me think how my CI always emphasizes how important it is that we get a good picture of the sacral spine with that upsweep and a prominent skin line. We don't want to accidentally scan the fetus and make it seem like the spine abruptly ends, when actuality it doesn't!
Hi Lania!
Yes, great point! I bet if we are off axis even just a little bit when scanning the spine it could make it seem like there isn't a sacrum!
Does your CI have any tips for you on how to get the perfect image of the sacrum?
Hi Brittany!
So today interestingly enough we discussed getting the sacrum as well as possible and my CI said it's literally all about small tilting and rocking movements of the transducer. These small movements make all the difference when trying to get that perfect sacrum as well as baby's position!
Hi Brittany,
I really enjoyed the images you shared as well as the information on Currarino syndrome! This week Dr. Wilson and I were discussing the importance of visualizing the skin line when obtaining our spine images and both pictures you included highlight that nicely. I noticed you mentioned this condition has a higher prevalence in diabetic mothers, why do you think that is?
Hi Chrishawna!
Excellent question. I also found it interesting that diabetic mothers were more likely to have a child with sacral agenesis. Through my research I found that there isn't a really clear answer for why this is. A few studies have been done and it looks like the hyperglycemic state of the mother with diabetes is what is impacting the development of the fetus.
One study said, "Poor glycaemic control periconceptually significantly increases the risk of fetal malformations" (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6516602/). I wish there was more information on exactly how hyperglycemia caused these defects but unfortunately there doesn't seem to be enough research yet.
My guess is that since the fetal environment is a very sensitive area that must be just right for development, the high glucose levels in the blood supply from the mother must be inhibiting the cells from differentiating and developing properly!
Hey Brittany! Wonderful post :)
I actually came here from someone's post on amelia, but realized what I was going to add was actually due to sacral agenesis. I follow a guy on TikTok (yes, they have educational videos too lol) that was born with sacral agenesis and ended up having to have both of his legs amputated because of it. His @ is spencer2thewest, and he makes a lot of videos about his life after the amputation and why it was necessary!
It's so sad to see these OB patients with deformities that we know will alter their lives once they are born, but I find it really inspiring when people overcome those challenges they face and can even educate the public on their condition!
Hi Lauren!
That's so sad that he had to have his legs amputated due to sacral agenesis. However, anatomically it does make sense... If a fetus doesn't develop a sacrum to hold the iliac bones together then I bet there isn't much stabilization / support for the lower limbs which could cause functional issues.
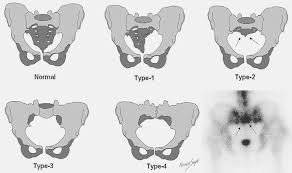
Here's a nice graphic I found that shows the different sacral agenesis types.
Good morning Brittany!
I found it so alarming when Allison discussed this topic during our lecture this week. A lot of the techs that I have watched always take multiple images of the spine and I never understood that... UNTIL NOW! Which is great and now I can't stop staring at the pattern of the spine-- making sure that it's symmetrical and normal in size and shape.
Great post and coverage on sacrum agenesis! Although I was just talking to my mom about how her cousin got diabetes when she was pregnant and then it was gone when the baby was born?? I wonder it this abnormality would still occur if the mother was recently diagnosed with diabetes... or only in mothers with ongoing diabetes? Hmmm, so much to learn next quarter!
Sounds like your mom's cousin had a case of gestational diabetes! This is when the mom develops diabetes while pregnant and it often dissipates after delivery. However, I was reading that if a woman gets gestational diabetes she is more likely to develop type 2 diabetes in the future! It makes more sense to me now why women with gestational diabetes, or just diabetes in general, are monitored so closely during pregnancy because the hyperglycemia can affect the babies development! Aka - sacral agenesis!
Here's a website that has some information on gestational diabetes and its symptoms :)
https://www.mayoclinic.org/diseases-conditions/gestational-diabetes/symptoms-causes/syc-20355339
Hey Brittany!
Thanks so much for responding back to me! That's so interesting to know about gestational diabetes and the whole development of womanhood-- shoot, that's a great back up excuse to pull when their kids grow up and wants to complain haha. I was discussing this abnormality with my CI and he was saying that sacral agenesis is typically prevalent with Type 1 diabetes!
Soooo much information, it's great to break it down with you guys.

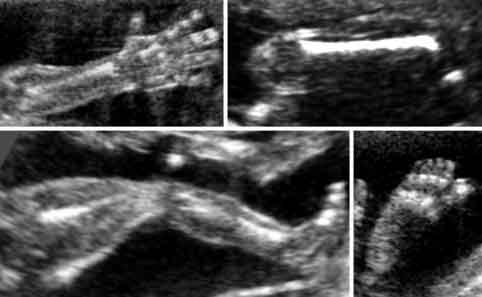
The image above demonstrates a normal representation of a tibia/fibula connected to a foot which is how it should appear while scanning a 20 week OB survey. It is normal because we see the side of the foot and it's properly attached to the distal tibia/fibula, but the bottom of the foot is not visualized as it would with clubbing.

This picture above demonstrates a clubbed foot (AKA Talipes), which is when you're scanning in a sagittal plane and it shows the shin bones (fibula and tibia) and you can see the bottom aspect of the foot. We shouldn't be able to see the bottom part of the foot, so when this is seen we can suspect clubbing is occurring and we would document this finding in our report to the radiologist.
Clubbed foot is a congenital deformity involving the foot and ankle giving rise to a plantar flexed, internally rotated and adducted foot. The incidence is about 1 in 1000 live births with a male to female ratio of 2:1. 50% cases are bilateral. Clubbed foot is a fairly common birth defect and usually is the only problem for an otherwise normal fetus. However, It may be associated with open neural tube defects, trisomy 18, or arthrogryposis. Surgery may be needed after birth to fix the clubbing or a doctor can perform treatment without needing surgery by trying both methods of: stretching and casting or stretching and taping.
Risk factors include:
- Family history. If either of the parents or their other children have had clubfoot, the baby is more likely to have it as well.
- Congenital conditions. In some cases, clubfoot can be associated with other abnormalities of the skeleton that are present at birth (congenital), such as spina bifida, a birth defect that occurs when the spine and spinal cord don't develop or close properly.
- Environment. Smoking during pregnancy can significantly increase the baby's risk of clubfoot.
- Not enough amniotic fluid during pregnancy. Too little of the fluid that surrounds the baby in the womb may increase the risk of clubfoot.
Hi Molly!
Great post and images!
I love how you incorporated the risk factors as well. That's important for us to know the history in the event we do find some sort of abnormality during our anatomy scan. Have you or any of the other ladies seen a fetus with club foot yet? I feel like I hear about babies having club foot quite often but I haven't personally seen a scan of a baby with one yet.
Hey Lania!
I think your post is great too! Thank you for explaining the most lethal form of skeletal dysplasia and the different types. Since it is lethal we will want to really embed this in our minds. The second image was a great example showing the narrow thorax with the abdomen protruding, resembling the champagne cork sign. That will be helpful with remembering. Little things like that really stick!
I haven't seen an officially confirmed clubbed foot in clinical yet, but last week there was a case I was scanning and I was having trouble getting images of the fetal legs (I think I shared this during our sharing circle Friday) and the tech couldn't visualize the legs well either from the baby's position. When they were finally able to see the feet, one of them looked like they could be clubbed, so they were going to have the patient come back for images of the feet. The foot just didn't look right, but they thought it was the baby's positioning. They didn't take the images of the foot, they felt more comfortable having her come back to hopefully get better images when baby is in a different position. A second tech also tried seeing the foot better, but neither could obtain optimal foot images. I will follow up with that case and see if a clubbed foot was actually determined or not.
Hi Molly,
Well done on such a thorough posting!! I liked that you included details on the sonographic appearance, risk factors, and other key details such as a higher prevalence in male fetuses. I was really curious about the treatment of this condition after the discussion we had with Dr. Wilson this afternoon. I recall her mentioning knowing someone around our age who had multiple surgeries to try to correct this problem. Although I am sure treatment is much better now than in the late 90's/early 2000's it sounds like it could take multiple surgeries to address this condition. I would love more information on how this condition is related to Spina Bfida, if you happen to stumble on an interesting article or video please feel free to share!
Hey Chrishawna!
I found a great article on a case report of club foot correction in child with spina bifida:
http://www.journalijar.com/uploads/526_IJAR-30738.pdf
It talks about the genetic, environmental factors, also the lack of folic acid playing a huge role in spina bifida. Also emphasized the most common deformity associated with spina bifida is clubbed foot.
The case study shared in this article is on a little 5YO girl who's mom actually took folic acid treatment prior to pregnancy, she was diagnosed antenatally at the level of L5, and at birth it was associated with bilateral clubbed foot. Also, interestingly enough there is no family history of spina bifida. Multiple surgeries were performed and they were able to help the patient without creating bone shortening.
Hey Molly,
Great response! I really appreciate how informative it is. I didn't know 50% of cases are bilateral. I think it makes a lot of sense club foot is associated with oligohydramnios, since amniotic fluid contributes so much to development. I have yet to get the chance to scan tibia, fibula or feet on the fetus. I am looking forward to getting practice with it though. Have you gotten practice scanning this anatomy? Also have you seen club foot in your clinical experience so far?
Hey Nailiah!
The anomalies we each wrote about relate quite well to one another! Your post is wonderful! It's interesting how for both rocker bottom and clubbed foot they start with trying to treat the patient using braces prior to doing surgery. I haven't seen an official diagnosis of clubbed foot, but one was suspected by my CI last week because they were having trouble visualizing the foot. Two different techs tried and were unsuccessful in seeing the foot appropriately from the side and it being attached to the tibia/fibula. It was appearing turned, but the techs were unsure if it was from the baby's position and didn't feel comfortable taking the images since they weren't a clear representation. The patient is scheduled to return and I am looking forward to finding out if the foot was clubbed or not!
As far as imaging the feet and other limbs, I actually practiced scanning the femur today on a 3rd trimester case that was being seen because her baby was measuring bigger than gestational age. It was challenging getting the femur horizontal across the screen! I was able to get the femur in view, but it was angled downward on the screen, so the tech I was with today told me to stay on the femur, but to carefully with minimal movement slide the probe up and angle downward to see the femur straight across the screen. I was able to get it and measure the femur twice, but it took some time struggling to get it that's for sure. The patients are always super understanding that I'm training and I always make sure to tell them before the exam that I'll be practicing scanning and the tech will be helping me.
Have you seen any clubbing or rocker bottom in clinics? What are you working on now with scanning OB's? I love how we can all share our experiences :)
Hope you had a great day at clinic! I had to get a coffee afterwards or else I would definitely be asleep right now. All of the critical thinking throughout the day and trying to retain all this new info is challenging for sure! I try to remind myself daily how blessed we all are to be here and working in the right direction to becoming great sonographer's! We are almost there.
Keep up the good work!
Hey Molly,
I also think that it is interesting that casts are initially used for prior to surgery. I appreciated that though, these babies are way too small to undergo surgery. Unfortunately in some cases they have too, but the less surgical procedures the better in my eyes.
Congratulations on getting that femur bone! I am so happy you're learning techniques to get the best images you can. I am interested to hear if that patient had club foot or not as well.
As far as my OB scanning I have been allowed to get measurements for the most part of like the cervix and abdominal circumference. I also get heart rate and placenta pictures. Today I was actually able to get the BPD/HC and femur bone with measurements, as well as the cord insertion on the abdomen which was nice. I only got to do it once though so I am hoping to get them again. Doesn't really feel like an achievement just yet.
I hear you Molly girl the balance is definitely a struggle.I definitely agree it is hard to absorb all the information. Hang in there!
Hey Naiiah!
Your're so sweet, thank you! It felt good to get the femur bone horizontal across that screen when I finally got it because it was super hard to obtain lol. It'll take time to get really good at it, but practice and more practice is key for us all! I'll keep you posted about the twin with suspected clubbing. Hoping her return appt is soon.
Awesome that you got to scan and take measurements of all of that today Nailiah!! It's great to get the practice in because its hard to obtain a lot of the OB images. I agree it doesn't feel like much of an achievement yet because my technique of getting many of the images needs to be worked on, but we're working hard at getting better! Super proud of you! It sounds like this week is going well! Stay strong!
I know this is a super basic intro to scanning OB, but I found this video to be helpful to me as a friendly reminder to start with a longitudinal sweep towards the mothers head instead of going straight into the uterus cine images from right to left and then transverse uterus cine images from superior to inferior. This way it'll really help determine baby lie and provide guidance of where to go to get those anatomy images.
https://www.youtube.com/watch?v=DVdP7cpovq8
Hi Molly,
It is so crazy that we learned about this yesterday in lecture, and then today in clinicals I saw bilateral club feet on a 20-week scan! Of all the possible pathologies though, at least this one has a treatment option. Thankfully there aren't usually other concurrent problems for the fetus.
Hey Leah!
Wow that's crazy you saw clubbed feet today! I am relieved that clubbed feet is treatable with either braces or surgery. That's great news nothing else seemed to be wrong with the baby. I wonder if clubbed feet runs in the mothers/dads family. It's definitely one thing to study these anomalies, but to see them in person is super sad! A tech showed me a twin OB scan she did over the weekend and one of the twins had dandy walker syndrome. The other twin was completely fine. We are in such a challenging and at times sad field when seeing these anomalies, but to know we can catch these anomalies so the parents can mentally and physically prepare prior to delivery is amazing.
Thank you for sharing!
Hi Molly! So much good info - great job! I found this video showing a live scan of a club foot and other abnormalities (start at 5:50 for the club foot). Since you've seen a potential club foot in the clinic, is this case a little more definitive than the one you saw?
Hey Alexis!
Such a great video demonstrating clubbed foot! Thank you for sharing! The twin's foot that had the potential clubbing wasn't definitive like in the video. The foot was slightly turned and baby wasn't in a good position said the sonographer's. That patient hasn't returned yet, but I can't wait to follow up and see if the techs can image the feet better next time around and if they can confirm/deny clubbing.
Loving all of these great visuals everyone's sharing!
Great work!
Hi Ladies!
I'll be discussing Thanatophoric Dysplasia! As I mentioned in my presentation earlier, it unfortunately is the most common form of lethal skeletal dysplasia. There are two types. Type 1 being associated with extreme rhizomelia, bowed long bones, and frontal bossing (prominent forehead). Type 2 is associated with straighter long bones, taller vertebral bodies, and Kleeblattschadel(cloverleaf skull). We also would notice sonographically as narrow thorax with a protruding abdomen giving it a "champagne cork appearance."
The first image is a normal profile image of a fetus.

This second image is an abnormal profile of a fetus with Thanatophoric Dysplasia, you can clearly see the frontal bossing and "champagne cork" appearance of the abdomen.

Hi Lania,
Great job on both your post and your presentation today!! Something about hearing my classmates explain a topic has always helped it stick with me. I was intrigued by the name of this condition so I looked up "Thanat" on a medical dictionary site and it turns out it means "death". This makes perfect sense considering this is one of the fatal types of skeletal dysplasias. I am wondering what specifically makes type 1 of this condition deadly? I know you mentioned several anomalies that this condition presents with but it doesn't seem like they are normally fatal on their own? Also really liked your mention of the "champagne cork" appearance, I could picture what you were describing instantly!
Hi Chrishawna!
Thank you love! But yes, in greek it means "death bearing" which like you said makes sense since it is lethal. But actually Type 1 and Type 2 are both lethal, they're both associated with pulmonary hypoplasia which unfortunately makes this condition deadly for these little babies. :(
Hey Lania great job!
I loved reading your post after I read up on cloverleaf skull for my DB, because as you mentioned, our topics are related! Cloverleaf skull is one of the many characteristics seen in Thanatophoric Dysplasia. I think I better understand now why skeletal anomalies are difficult to diagnose before birth, since many characteristics can be associated with different diagnoses. I found these images also helpful! It's a very sad diagnoses, since it's lethal as you mentioned.


Hi Zuly!
Yes! Our topics were definitely related and I so agree with you that they can be hard to diagnose because these babies can have multiple different issues all due to one skeletal anomaly! It breaks my heart to know that these babies are born with such terrible dysplasia. :( Thank you for sharing these images as well though!
Cloverleaf skull
(aka Kleeblattschädel syndrome or deformity)
Cloverleaf skull is a rare genetic disorder and a type of craniosynostosis (birth defect in which several sutures in the skull fuse too early). It results in the skull having a cloverleaf shape from bulging at the front and sides of the skull. The sutures involved are typically the sagittal, coronal and lambdoid sutures. Most patients with cloverleaf skulls have intellectual impairment and hydrocephalus (excess cerebrospinal fluid build up within the ventricles of the brain.)

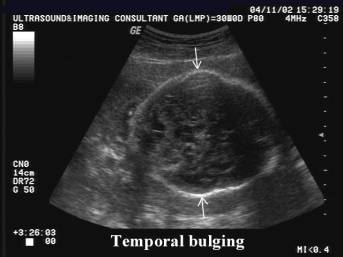
- On the left we can see a normal fetal skull. We know it’s normal because the bones are continuous and smooth, the skull has an evenly ovoid/rounded shape. We can see the bone in the anterior aspect causing some artifact, making the cerebral structures a little more difficult to visualize than the posterior side. This is a normal finding, letting us know the one mineralization is as it should be.
- The middle image demonstrates a cloverleaf skull. We can observe the bulging at the front and sides. The shape of the skull is no longer smooth and evenly ovoid/rounded.
- The image on the right demonstrates a more subtle cloverleaf presentation, we can observe the temporal bulging.
Cloverleaf skull is usually seen in the context of the following condtitions:
1. Thanatophoric dysplasia (typically type II only)
2. Severe Apert syndrome
3. Severe Crouzon syndrome
4. Boston-type craniosynostosis
5. Carpenter syndrome
Hi Zuly,
The differences between the first and second images you shared are insane, but a great representation of your chosen anomaly! I love that you mentioned the artifacts we typically encounter in a normal skull, so lack of those should indicate an abnormality. Since it can be associated with thanatropic dysplasia is this condition usually fatal or would it depend on the severity of the deformation. I am also wondering how we would take our normal biometry in this instance, perhaps we could use the "trace" tool to outline the skull for our HC or if a sonographer wouldn't bother because maybe it's too inaccurate? Curious to hear your thoughts on this! :)
Hey Chrishawna!
Thank you for this great question. I couldn't find any real information on measuring cloverleaf skull, but I like your idea of using the trace function! Maybe a BPD would be taken at the most narrow and at the widest portions as well? I imagine once cloverleaf skull is seen on ultrasound, that part of the protocol is adjusted in some way to provide more useful information. Or maybe this part of the protocol would be excluded all together like you mentioned!
Hi Zuly!
It's interesting to see that the cloverleaf skull is a rare genetic disorder and fetal development. I don't know why assumed that abnormalities can be one or another. If it is genetic, I'm also assuming that this gene is recessive? The images that you shared showed great examples of the different extent of this abnormality that I never knew about. It's important to be aware about how different these abnormalities can look, but I could definitely tell (last image of temporal bulging) that the fetal skull does not look normal! Great description about the normal fetal skull, as well. Noticing the hyperechoic, ovoid structure, and it's ossification is highly important!
Hope you get some OB today at clinicals! I love being able to reflect after our Monday class.
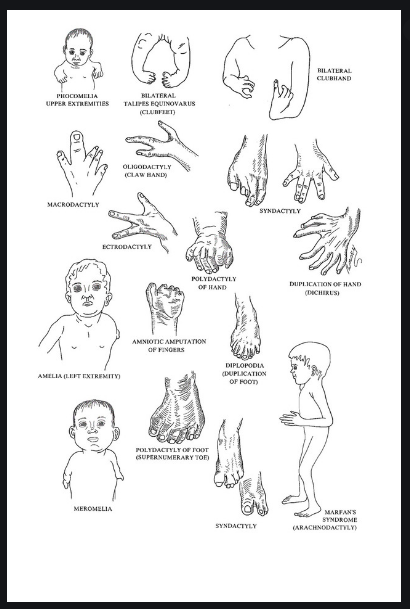
Congenital vertical talus (more commonly known as rocker bottom foot) is an anomaly that is a result of malposition of the talus bone during development. Essentially the talus bone forms in the wrong position, which causes the bones in front of the talus to shift on top of the talus. A rocker bottom would foot will be very flat oppose to having that concave appearance that gives the foot its arch. Also the calcaneus (heel) will be protrude more posteriorly and curve outward.The foot essentially looks like the bottom of rocking chair. Congenital vertical talus should be treated early or the child will experience difficulty walking accompanied with pain. Non-surgical treatment is generally attempted first. This consists of stretching and special casts. If the noninvasive attempt is unsuccessful surgery will be performed.
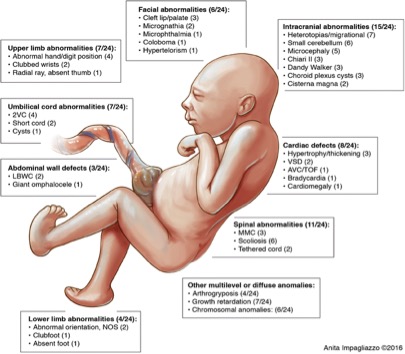
I found an image that depicts other anomalies that could be present with rocker bottom.
This website also has some awesome images on skeletal dysplasia in general:
https://www.slideshare.net/padmanishailesh/congenitalskeletaldysplasia-seminar-shailesh

Hi Nailah,
I love the resources and images you shared, especially the little baby with multiple conditions. One thing I like about your chosen topic is that it looks the same in real life as it does with sonography so it's easier to wrap my brain around. I was looking online to see if I could find detailed pictures of the bones of the foot so I could understand their unusual arrangement in rocker bottom feet. I stumbled on a cool graphic that was labeled charcot foot and it seems to be similar to rocker bottom! Do you know if this condition is usually bilateral or unilateral and if it occurs sporadically or is genetic?
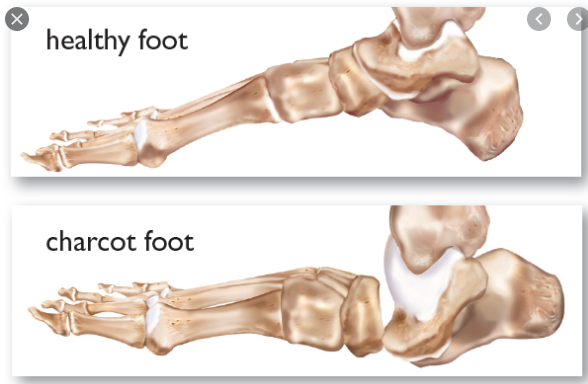
Hey Chrishawna,
I agree I appreciate how I am able to understand this anomaly more based on the similarity in sonographic and physical appearance. Thank you for sharing those images I appreciate that. I was looking into bones of the feet as well as I was developing my response. I found that rocker bottom may also be associated with dorsal and lateral dislocation of the talonavicular joint. I just didn't totally understand it to where I could explain it well and I didn't want to confuse anyone.
This is the joint here:
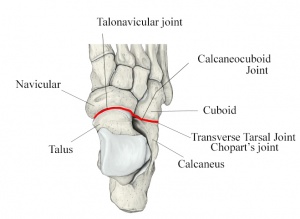
Hey Nailah,
Great post. This one for sure confused me a bit on what was actually abnormal. I know the sonographic image will show a rocker bottom foot but I didn't fully understand why it would look that way. However, you explained it very well. I thought this image was a good representation of how the talus is misplaced and the other bones are shifted closely to the talus.
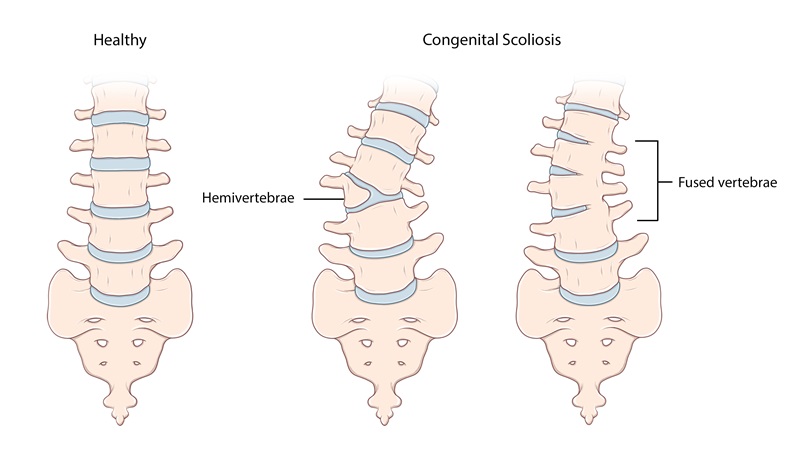
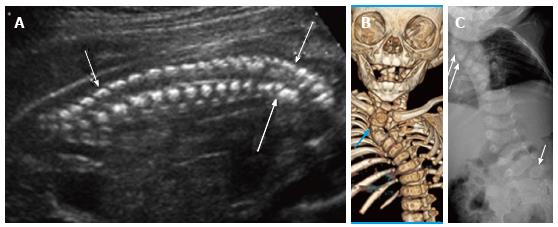
This is the normal fetal spine. It is normal because all ossification centers are present and in the correct anatomical location, there is asymmetry between all vertebra, the spine shows slight convex and concave shape, the sacrum is pointed posteriorly and present.

Here is an abnormal spine that is demonstration a hemivertebrae. This is a condition where half of the vertebra in the spine does not form. The cause of a hemivertebrae is unknown however some suggest its probable cause is lack of blood supply to the vertebrae. Sonographic assessment will demonstrate a "kink" in the spine which makes the contour look off. You may also notice a wedge shaped vertebra only on a single side. Hemivertebrae can express itself as kyphosis, scoliosis and lordosis


Hi Allison,
These pictures are incredible and I appreciate that you included a representative image in all three scan planes, its really helpful to see it this why while were still getting this concept down! The spine is one of my favorite images to see when I observe OB, something about the shape and symmetry is so appealing to the eye. Apparently a hemivertebrae can be corrected surgically in infancy by removing it and then fusing the superior and inferior vertebrae together! Do you think this condition could be caused by a malformation in the mesoderm or maybe from an outside factor like maternal teratogens? I remember in your presentation you mentioned the importance of Folate during pregnancy, especially for the development of the spine, do you think a lack of folate could be the responsible?
Hey Chrishawna,
After researching it more. I it seems to be unknown why hemivertebraes occur. One source said it could be due to a lack of blood supply to the vertebra so it never fully proliferates because it isn't being fed enough to grow. Another said it could be congenital, which corresponds to what Dr. Wilson has said about family history playing a large role in skeletal dysplasias. Also I believe any teratogens can cause any malformation with a fetus.
As for folate. Folate is really important for the cell proliferation process ( dividing, folding & fusing) of the neural tube. The neural tube is formed by the ectoderm whereas the vertebrae is formed by the mesoderm. So for folate I think it is beneficial for the neural tube not necessarily the spine formation.
Awesome job Allison!! Thank you for the clarification on the folate, I knew it was important, but couldn't remember for what exactly! :)
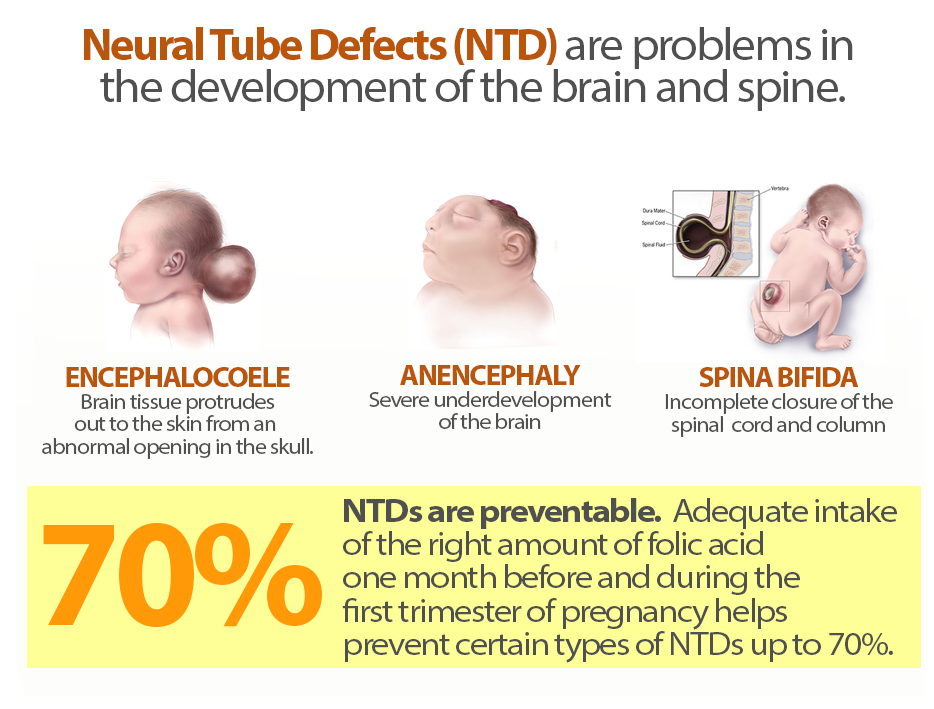
Great post Allison! Crishawna I was also a bit fuzzy on the folate association. I liked these images, I think spina bifida is the one Michelle mentioned in class? It's incredible these can be prevented with taking enough folate, I found this page from the CDC very informative regarding it's importance in pregnant women, and I liked that it points out neural tube defects occur in the first few weeks of pregnancy, so it's important to take folate before!
Zuly,
These are great! Yes my mind was blown when I found out the neural tube forms in 2-4 days in the 5th week of pregnancy. Some women may not even know they are pregnant yet!!! Folate can decrease NTD by 70%. So Folate, Folate, Folate!! Also another random fact is that folate is better to have than the synthetic version aka folic acid. Apparently some women with certain gene mutation (MTHFR) can't actually absorb folic acid so they must take folate!
Hi Allison,
I liked your pictures and can see the differentiation from the normal vertebra compared to a hemivertebrae. However, I remember Dr. WIlson showing the image in lecture that was super discrete and difficult to point out which makes me scared. I also did not know that kyphosis and scoliosis is apart of hemivertebrae.
Hey Candee,
Yes it can totally be discrete! So many little bones that need to be perfectly shaped and in the proper location! This is why it is so important to scan the spine in all 3 scanning planes. In this image below you can see the coronal scan plane (lateral hemivertebra) can show different pathologies than the sagittal (Dorsal hemivertebra).

Hey Allison,
This response was great. I really appreciated how the normal images broke down the 3 ossification centers. I am still struggling with the fetal spine. I think I can tell if something is abnormal, like if it shaped weird. I am still confused on if we should just be looking if the spine appears abnormal in sagittal view or is there something we should be counting as well. Also how obtaining the views of the vertebral body vs posterior processes are different.
Nice work!
This site has some spine anatomy. It as discusses lordosis, kyphosis, and scoliosis.
https://courses.lumenlearning.com/nemcc-ap/chapter/the-vertebral-column/
Also here is a nice fetal spine depicting intact skin really well.

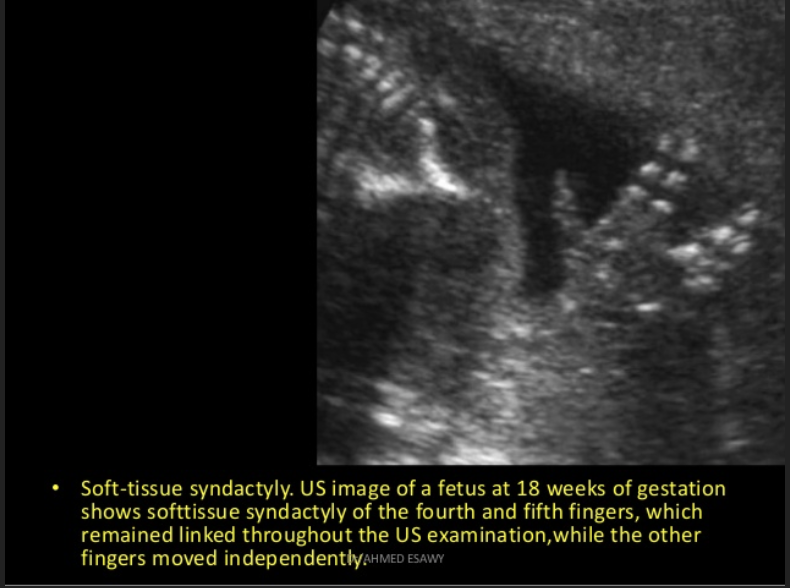
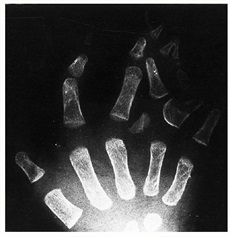
Below is an image of a normal fetal hand. In this image, you can see the three ossified phalanges of the long fingers and the two ossified phalanges of the thumb. It would also be normal to see the 5 ossified metacarpal bones. The carpal bones are hypoechoic and will ossify after birth. The hand and fingers appear to be in a neutral position, but in real time we'll want to see them in spontaneous motion, including in flexion and extension. If we see a hand that is clenched into a fist, we'll want to circle back to it to see if the hand opens.

Below is an image of an abnormal hand, specifically with syndactyly. Syndactyly is the fusion of soft tissue or bony segments of fetal digits. In this image, the fourth and fifth finger appear connected. There is little3 space seen between the fingers, unlike the normal second and third fingers. As the image caption states, the normal fingers moved independently in real time whereas the fourth and fifth fingers exhibited conjoined movement. Sydactyly can occur in the digits of the hands and feet.
During the formation of the hands, the hands will initially develop as paddle-like structures. Later the fingers will separate. The failure to separate causes syndactyly. It can occur as an isolated event or can be associated with other anomalies or syndromes. Both genetic and environmental factors seem to play a role in its occurrence. It is associated with triploidy, acrocephalosyndactyly syndromes, and Down syndrome to name a few.
Excellent post Alexis! I like how you highlighted the real-time findings that should be observed as well. It made me think of arthogryposis which presents as contractures with restricted or non-existent joint mobility.
https://www.youtube.com/watch?v=9tYhX14g1ew
This video clip shows in real-time how the joints are unmoving and abnormally flexed.
Hi Alexis,
You did a fantastic job on this posting! I think the images you shared do a great job of representing your anomaly. Is this condition typically seen bilaterally when it occurs, or if it is seen in a fetal hand is it there a higher chance of it developing in the feet?
Great question, Chrishawna! It seems syndactyly occurs bilaterally in 50% of cases and is more common in males according to this article. The article also does a fantastic job explaining the embryology of the fetal hand and also how it can be surgically correct.
In regards to your second question, I couldn't find a statistic of how often both hands and feet are affected by syndactyly so I'm not sure if there is a correlation. Both hands and feet seem to develop at the same time, but I would imagine their gene expression is different. Perhaps they're not both affected unless there was an underlying genetic issue spread across the genes for both. It would be an interesting tidbit of information though!
Hi Alexis,
I gave you such a difficult question and you did a marvelous job at answering it!! I really enjoyed the article you shared, it had so much information on the topic and was pretty easy to follow for the most part. Heres an image from the article I really liked, I couldn't imaging trying to surgically correct a case like this!
This week I did a little research on Asphyxiating Thoracic Dystrophy (aka Jeune Syndrome). One of my primary resources was the National Organization for Rare Diseases (NORD)
Below illustrates what we normally see in a health fetus.
THORAX - we see the ribs curving out around a normal sized chest with lungs and heart each occupying approx 1/3 of the area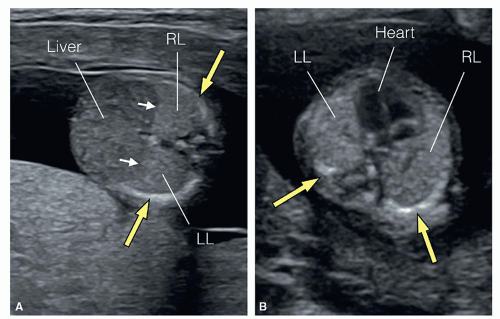
FEMUR - appropriate length, appropriately ossified, not bowed
Asphyxiating Thoracic Dystrophy (ATD) is an exceptionally rare type of skeletal dysplasia that primarily impacts fetal thoracic development. This finding is sometimes called a "bell-shaped chest" (image below). This is problematic as it can affect lung development and result in pulmonary hypoplasia. Additional findings include 1) shortened limbs, 2) polydactyly, 3) short stature, and 4) kidney issues due to renal cyst development.
ATD is autosomal recessive, meaning that both parents need to be genetic carriers. According to NORD, there are 24 genetic mutations that have been identified as a cause of ATD. As previously stated, it is rare disorder with an incidence rate of 1 in 100,000-150,000, and appears to affect males and females equally. Outcome can be extremely severe, but from what I can tell ATD is not classified as uniformly fatal.
ABNORMAL THORAX - abnormally small in size with short ribs; second image illustrates a common finding in ATD called "bell-shaped chest"

FEMUR - shortened
ATD

Hi Leah,
Thank you for sharing your resources it looks like that site had awesome information on ATD. As I was reading your posting about how the condition presents it reminded of the characteris tics sometimes seen with dwarfism. Do you know if these two conditions have any relation?
Hi Chrishawna! Great question.
Multiple sites stated that ATD is a form of dwarfism, or that the resulting clinical presentation of ATD would qualify as dwarfism, so I think it is fair to say they are pretty closely related. I was a little unclear if they are the categorically the same or if one is caused by the other. I'm sure it will all become much more clear next quarter when we dive into pathology.
Hello everyone!
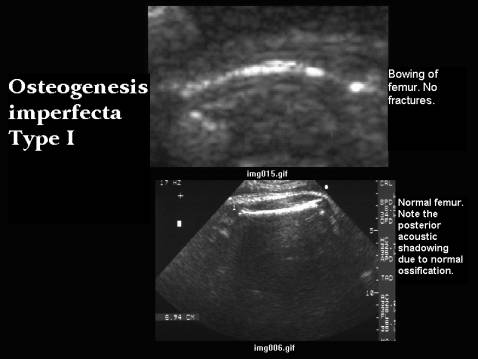
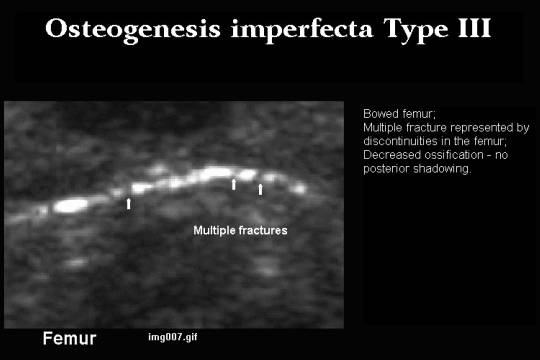
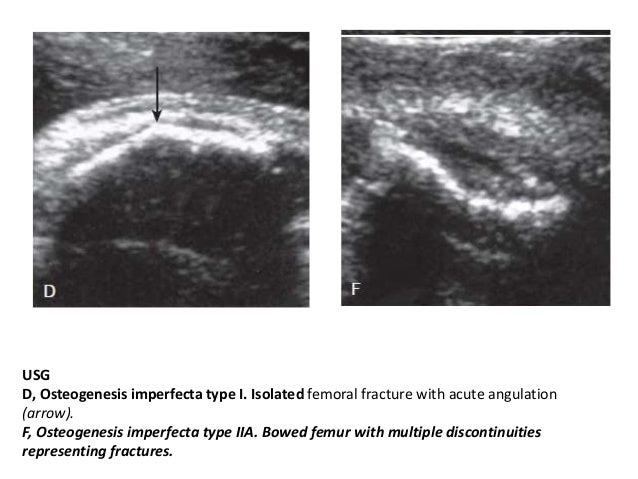
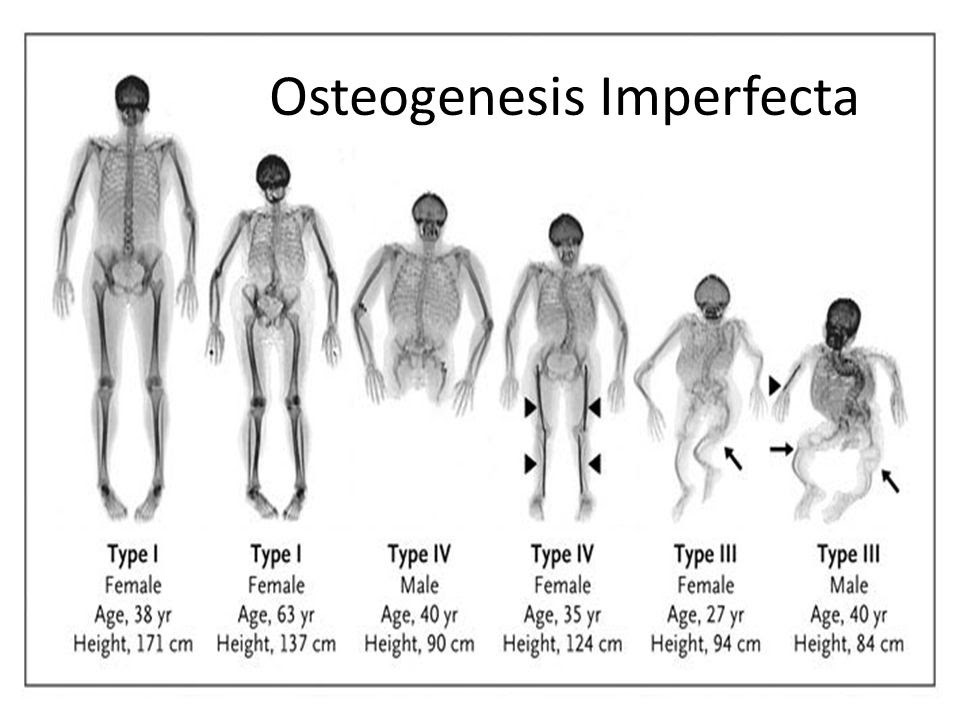
I decided to do osteogenesis imperfecta. It's a group of genetic disorders that mainly affect the bones. Osteogenesis imperfecta means "imperfect bone formation" People with this condition have bones that break or fracture easily, often from mild trauma or with no apparent cause. In this first image, it shows a comparison between the normal femur, this image shows good ossification and we know this by the shadowing thats present and no bowing with a good length. Compared to the image above that which shows type 1 osteogenesis imperfecta with bowing and it doesn't show the good ossification we see in normal.
There 8 types:
Type 1: Mildest and most common type. About 50% of all affected children have this type. There are few fractures and deformities
Type 2: Most severe type. A baby has very short arms and legs, a small chest, and soft skull. They may be born with fractured bones. They may also have a low birth weight and lungs that are not well developed. A baby with type II usually dies within weeks of birth
Type 3: Most severe type in babies who don’t die as newborns. At birth, a baby may have slightly shorter arms and legs than normal and arm, leg, and rib fractures. A baby may also have a larger than normal head, a triangle-shaped face, a deformed chest and spine, and breathing and swallowing problems. These symptoms are different in each baby
Type 4: Symptoms are between mild and severe. A baby with type IV may be diagnosed at birth. They may not have any fractures until crawling or walking. The bones of the arms and legs may not be straight. He or she may not grow normally.
Type 5: Similar to type IV. Symptoms may be medium to severe. It is common to have enlarged thickened areas (hypertrophic calluses) in the areas where large bones are fractured
Type 6: Very rare. Symptoms are medium. Similar to type IV
Type7: May be like type IV or type II. It is common to have shorter than normal height. Also common to have shorter than normal upper arm and thighbones.
Type 8: Similar to types II and III. Very soft bones and severe growth problems.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteogenesis-imperfecta
Hi Hailey!
Osteogenesis imperfecta is such a sad anomaly. It breaks my heart to think of the fetus constantly fracturing a new part of its body.
I actually first learned about this condition through Grey's Anatomy and it really helped me remember it! In the show, one couple is having an ultrasound on their baby and the doctor doing the scan finds that the baby seems to be sitting cross legged. The parents thought this was cute and noted that their baby was doing this on their last ultrasound. They referred to the baby as their "little Buddha" because of his positioning.
However, this raised a red flag for the doctor, as it should for us as well. The baby had been in this position for a long time and didn't show signs of moving. This led to more tests which found that the baby did in fact have osteogenesis imperfecta. The baby was likely not just sitting cross legged but actually had broken legs and couldn't move them. :(
This reminded me how important it is to check the previous exams and images for comparison. We need to watch for cases like this where the baby isn't showing signs of movement, or their bones seem oddly positioned, as they could be fractured.
Oh my gosh Brittany! I'm going to have to look that episode up! but yes it is extremely sad. We really have to make sure we notice these things and not get stuck on just visualizing one thing like the heart like Dr. Wilson said. I remember her saying if you find an anomaly that's great, but don't get stuck on it and dismiss the rest of the fetal body, there can be multiple issue going on. History is so incredibly important! this reminds me of a time in clinic where my CI told me to go start a pelvic exam. I'm not told any history usually (which sucks) so I go head and start and I'm looking for the uterus forever! Eventually my CI comes in and she says "so when was your uterus removed" I was pissed to say the least LOL! instead of searching forever I should have gotten my own history and asked the patient if she had any prior surgeries. Ive learned my lesson!
Aww I bet that was frustrating!
History is definitely super important. I think the timing of asking for history is also a key factor. Like Dr. Wilson said, it's usually best to ask about patient / family history before even setting the probe on the patient. This way they don't think you're asking these questions because you see a certain pathology during the scan.
I'm also a bit curious about the cultural aspect of certain skeletal dysplasias, like dwarfism for example. The most common type of dwarfism is rhizomelic dwarfism and it results from achondroplasia. While this genetic disorder may be upsetting for us to find as sonographers, I wonder if it wouldn't be this way for the parents if they also have dwarfism. To them it may be exciting to have a child that looks like them.
I experienced this situation when I was learning sign language in high school and engaging with the Deaf community. Many of the Deaf parents explained that they had Deaf children as well, and while their doctors were upset, they were actually thrilled! The parents saw it as a unique difference, and even went as far as to call deafness a blessing.
These cultural aspects may be something we have to look out for and learn to navigate when we see certain pathologies.
Hi Hailey,
I love how in depth your posting is, you already sound like an expert on this topic!:)
The first OB exam I ever observed the baby had a femur that looked exactly like the picture you shared (image D). We didn’t know it at the time, but it turns out the patient had a previous pregnancy where the baby also had skeletal dysplasia, so the report said mom was not surprised that this baby had it too!
I am wondering how the condition compares to brittle bones where patients present with bone weakness and are easily broken?
LOL definitely not an expert! there was just so much to learn when I was researching it. That's so crazy that you saw that and really good exposure! I can't wait to start doing OB, I was just telling a tech today that I wish we did more of it. I'm not sure I totally understand the question lol I looked up conditions that causes weak bones and osteoporosis and osteopenia came up. I think brittle and weak bones are in the same category though.
Hi Hailey
Very interesting post, know we talked about osteogenesis imperfecta but it didn't occur to me that it would look like this on ultrasound. I was wondering if it had to do with the composition of the bones and whether the mother took folic acid during her pregnancy. I also wonder if this affects whether the bones are echogenic or not echogenic. Do you know how osteogenesis imperfecta occurs?
Hi Candee,
I found this article that goes into how OI occurs and it mentions that it's caused by defects in or related to a protein called type 1 collagen, ollagen is an essential building block of the body. The body uses type 1 collagen to make bones strong and to build tendons, ligaments, teeth, and the whites of the eyes. The remaining cases of OI (types VI–XI) are caused by autosomal recessive mutations in any of six genes (SERPINF1, CRTAP, LEPRE1, PPIB, SERPINH1, and FKBP10) that code for proteins that help make collagen. These gene changes are inherited, or passed down from parents to their children; people who have OI are born with it. However, in some cases, the gene mutation is not inherited and occurs after conception.
So it looks like it can be inherited but sometimes not!
Amazing job on your post Hailey! You did such a great job explaining it. I found this page that goes over an OB case that was found to have osteogenesis imperfecta type II. It has some great images including this one demonstrating the small chest that may be present as you mentioned and also one of shortened and fractured ribs. The clinical history of the patient is as follows:
"We report the case of a planned pregnancy in a healthy 36-year-old woman. There was a prior uncomplicated pregnancy that gave rise to a healthy child. There was no consanguinity, no family history of previous disease. There were no known exposures to any teratogens. Folic acid supplementation was initiated pre-conception." I thought it was great they mentioned she started taking folic acid before conception, since Allison highlighted it's importance in her presentation!
https://www.eurorad.org/case/13376


Nice post, Hailey! It is quite interesting how wide the spectrum of severity is for OI. Makes me wonder how many people have the mild form of OI and don't even know it!
I found a YouTube video showing a case of OI (type unspecified), and the limb bones do look segmented. Seeing the discontinuity of the shadowing from the bones really caught my eye.
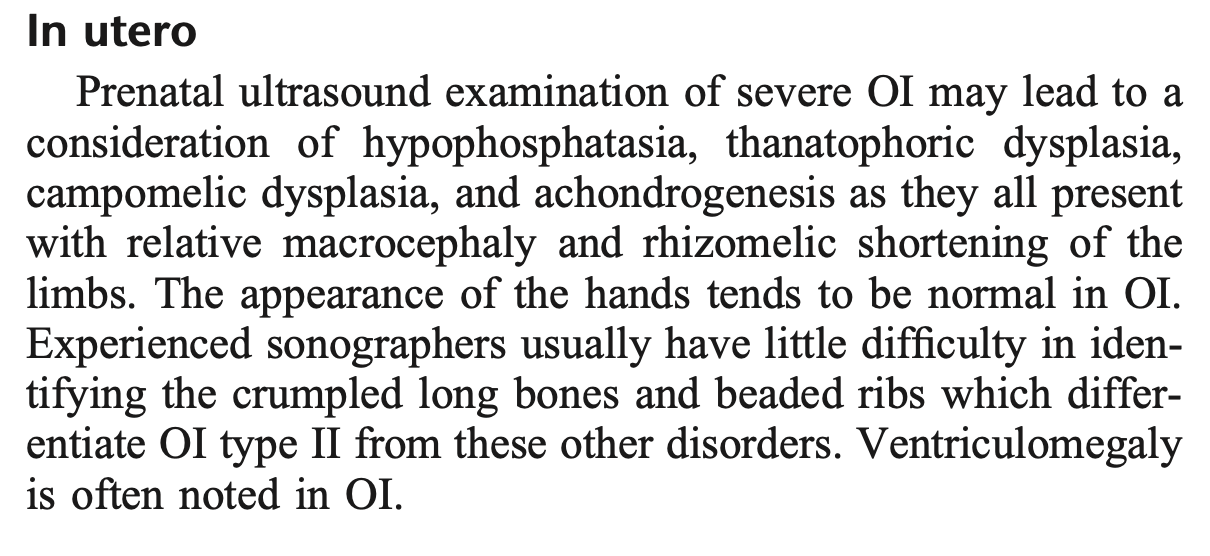
Also, below is a short description of some of the sonographic appearances of severe OI in a fetus. Seeing the number of differentials listed also reinforces the sentiment behind this DB. We don't need to determine exactly what condition the baby has (especially because there are around 400 skeletal dysplasia conditions!) - we just need to recognize when something is abnormal and document the best we can.
Hailey,
Yikes I bet these poor babies hurt. Here are a few helpful videos on osteogenesis imperfecta!
https://www.youtube.com/watch?v=JA5ap43iFrQ ---This is what OI is. Apparently the severe form can cause hearing loss. I guess that makes since because the mallus, incus, and stapes are bones.
https://www.youtube.com/watch?v=fI5ZRzDIOCk -----This is a humanized video.
Sarah
SO SORRY GUYS I meant to reply but I made a new topic instead.:( It's past my bedtime lol
Hello everyone,
As we all know, it is very important for us to not only get great pictures during OB scans but also look out for any abnormalities. One such abnormality that can get unnoticed if a sonographer is not paying attention is the lemon sign of the fetal skull. To recap, the fetal skull or calvarium should be smooth, bilaterally symmetrical, and usually of ovoid shape. The bone should be fairly echogenic and be continuous all around the circumference. We can see a normal skull in the picture below:

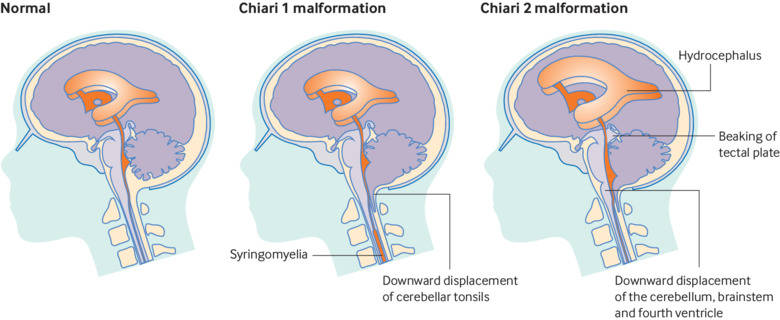
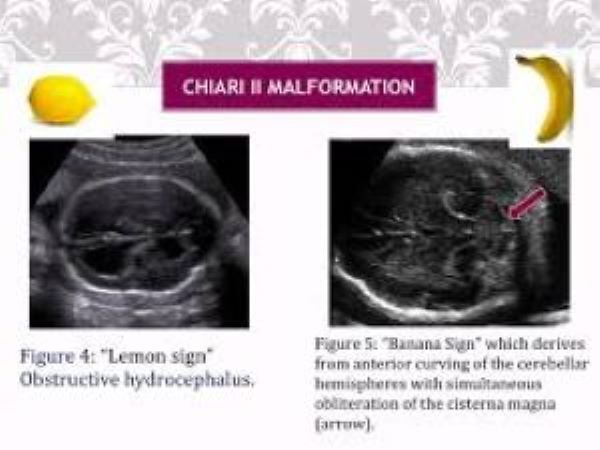
On the other hand, the lemon sign occurs when the frontal bones of the skull start to appear flattened or scalloped, giving the skull the shape of a lemon. The lemon sign has been linked to spina bifida for it is believed that a decrease in intraspinal pressure in fetuses with spina bifida causes the brain to shift downward. It is also a classic sign of Chiari II malformation.

https://radiopaedia.org/articles/lemon-sign-1?lang=us
https://pubs.rsna.org/doi/abs/10.1148/radiol.2281020448?journalCode=radiology
Hi Raman,
Nice job on your posting, it’s funny how many food references are used in the medical field! Have you seen any of the cranial conditions we’ve discussed in class at your clinical site? Also wondering how this condition can contribute to chiari II malformation?
Hi friends,
I feel like we are a close and respectful cohort so I feel comfortable sharing my own experience with this topic to help others understand better.
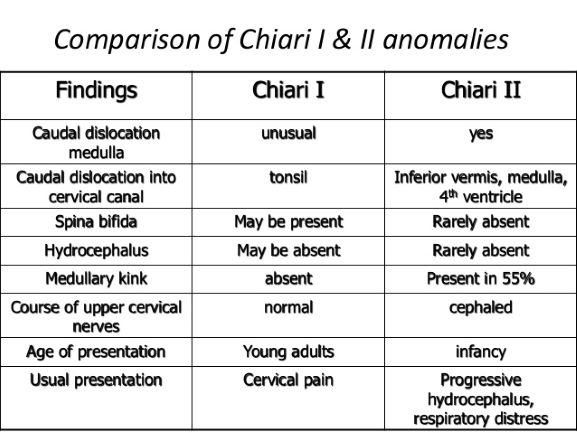
I actually have Chiari Malformation Type 1 and I wasn't diagnosed until adulthood, which is typical with this type. For me, my diagnosis came after years of suffering with constant headaches, neck tension, and feelings of pressure in my skull. Thankfully, I don't have any other more serious symptoms or functional issues.
Chiari headaches are so unlike typical tension headaches or migraines. It's a feeling of extreme pressure and tightness that no amount of pain medicine can help. They often stem from the backup of CSF flow in the brain. Since the cerebellum is herniated a bit too low into the foramen magnum and area of the brain stem, this can cause a blockage or back up of CSF flow leading to the feelings of pressure. There is a decompression surgery that can be done to alleviate symptoms, but this requires the removal of a part of the skull in the back of the head near the cerebellum to allow the brain more room, and months of recovery. However, sometimes when my headaches get really bad, this invasive surgery actually sounds really nice! The pressure makes you want to have some type of outlet so bad that even taking out some of your skull seems like a great idea!
I was diagnosed through MRI, whereas type 2 is usually diagnosed in babies with ultrasound when the findings of a lemon sign skull and a banana sign cerebellum are seen. Type 2 is also associated with spina bifida. I've attached an image below to show the different ultrasound signs seen with type 2 and a chart to show the differences between Chiari type 1 and 2.
I hope this helps give you all a little more insight into this condition and if you have more questions about my personal experiences from living with it, I'd be happy to share.
Hi Brittany and Chrishawna,
Firstly, thank you so much Brittany for sharing your condition with us. I am so sorry you have to deal with that and was wondering how do you best handle the symptoms since you said medicine does not help? And would you ever do the surgery? I looked up the MRIs just to see how they look like.
For lemon sign and Chiari II malformation, I could only find one resource to the state a possible reason they are related. Since the brain elements are moving downward, there is less pressure on the skull causing it to flatten instead of develop its normal shape. Kind of like when shaping clay we need to keep our hand to put pressure and create a shape. Without the pressure, the clay would just fold onto itself. Another way to think of it is that in Chiari II malformation, the brain matter is being pushed out of the foramen magnum, so its being squeezed out causing an indentation in the skull.
https://radiopaedia.org/cases/lemon-and-banana-sign?lang=us
Thank you both so much for the kind words.
For me, the symptoms are often triggered by stressful events and posture. I have to be careful when we are on Zoom all day and I'm looking down at my computer, or if I'm looking down reading for long periods of time, as these angles just compresses the already tight area in my brain stem even more which will trigger a headache. Stressful days with sensory overload will also trigger the symptoms.
I've tried muscle relaxers to release the tension and pain in my neck muscles, but honestly I didn't see much improvement. Usually my go to is an ice pack on the back of my head/neck area and laying down in a dark room until the symptoms pass. However, this isn't always doable when the headache starts in the middle of a work day! Haha. However, I've gotten pretty good at just pushing though and trying to manage my symptoms. Luckily for me the condition isn't debilitating and thankfully I have no cognitive or functional issues.
As far as the decompression surgery goes, I've talked with my neurosurgeon about it and it definitely seems scary! It requires removal of a piece of the skull and reattachment of the muscles in that area into new insertion sites on the skull. Typically patients have even worse headaches during the month of recovery, and it's possible the procedure won't help with their symptoms at all. For me, since my headaches can usually be managed, I'm holding off on surgery for now but may consider it in the future when I have time for the recovery period. It sure sounds nice to know what it feels like to not constantly have pressure in my head! Haha :)
I just want to thank you for sharing your personal experience with us Brittany! You are incredible for pushing through this program while managing your symptoms, you've got this!
Brittany,
Seriously amazing you sharing your personal experience with us! You are such a dedicated hard working student in this tough program despite the pain you endure. Truly inspiring! We are all here to root you on and provide support!! Thank you for sharing this information to educate us on the differences in the two types of chiari.
In a normal fetus, we see a chin not jutting out too far from the profile and also not deep to the profile. The website Dimensions of the fetal facial profile in normal pregnancy - Goldstein - 2010 - Ultrasound in Obstetrics & Gynecology - Wiley Online Library explains how normal facial/profile proportions are determined and why they look for those measurements. The following image shows the typical fetal facial profile, measuring a few different proportions (protrusions and concavities).

In our careers, however, we may come across a fetus with micrognathia, or mandibular hypoplasia. This will present as a profile with a small chin/jaw that does not protrude to the point it should. This may present as just a small chin in the profile view, or a lack of bottom lip present in the same plane as the nose and lip in the coronal view. Micrognathia may be inherited or can be caused by a number of genetic mutations such as Pierre Robin syndrome, trisomy 13 and 18, achondrogenesis, progeria, or Treacher Collins syndrome (healthlinecom). Good news is, often micrognathia corrects itself during growth, but if it doesn't, complications such as improper tooth alignment may continue throughout development after birth. The following image is from Radiopaedia showing extreme micrognathia:

Lauren,
I really like the image showing the measurements. I never really knew you could even measure those parts. Have you seen any anomalies that involved any part of the fetal face in clinic? If so what tips did you CI give you to properly document them?
Hi Allison! Thankfully I haven't come across any facial anomalies yet, but I did have a patient that had a previous trisomy 13 pregnancy so I was worried her new babies' 20-week scan would show an abnormality. My CI does get a ton of profile pictures both for diagnostic reasons and for the parents to take home and pictures of the nose and lips so assess those areas.
Hi Lauren,
I had to double take when I looked at the second photo showing micrognathia, at first I was unsure exactly what I was seeing! Like Allison mentioned, I had no idea that some institutions take these measurements, but it seems you can measure just about anything. Do you think microganthia may be more common in ethnicities that tend to have smaller proportions? Also wondering if the same is true about the measurements taken in the first image. I think of my own family and how different their physical traits are. My dad's side of the family has a much wider nose, larger eyes, and fuller lips compared to my mom's side and all of my dad's brothers share this trait.
Nice post, Lauren! That's great news that micrognathia tends to correct itself with time. I found this short live scan video showing the profile of a fetus with micrognathia. I think watching a live video helps me lock it in so I thought I would share! I also saw some other videos in my search showing the corrective surgeries for micrognathia and the results are amazing!
Hello Lauren! You've completed the concept of abnormality of micrognathia really well. I have been finding that most abnormalities have different severities, which confuses me, BUT then you mention what genetic mutation occurs & it's sometimes different. I know that if it's one thing gone wrong, there's another abnormality (around the development of the Brain?) It's so interesting to find that it can actually fix itself during development!! That's really nice to know after all these other different pathologies that we're going over.
Thanks for also sharing the great images and resources that indicates how to measure the fetal face! Really awesome post.
Hi Lauren,
Great job on this post! Yet another abnormality that is so easy to miss, especially with mother's body habitus, fetal lie, and the fact that baby is moving around!!
I think there comes a point in pregnancy where a sonographer really needs to take the full time allotted to make sure they capture everything (with ALARA in mind) just so we don't miss ssomething... or at least, I think there should be.
Thanks!
Karen
Yes! You mentioned maternal body habitus affecting our image quality - the BMI 58 patient I shared about last week actually was our patient again today for a recall on most of the anatomy images. I just kept wondering the whole time I was observing that even with my CI trying her best to get these views, they still weren't great. What do we do then? And this is only her 20 week scan, so I imagine that it will only become more difficult to see once baby's head and other bones continue to develop more. I feel sorry for these patients because they are high risk already and then we can't get the optimal pictures we need to catch any fetal abnormalities :(
As our class is discussing different anomalies, I chose to do the radius! During a normal fetal ultrasound of the hand, you would see five hyperechoic/ cylindric metacarpal bones, its independent digits of different length, and a normal radius, ulna (lateral to the radius), and humerus (head is distal to the radius). During the ultrasound, we should also see, from time to time, that the fetus is able to flex and extend the fingers and wrist. Images below are fetal ultrasounds of the normal fetal hand.
Radial ray anomaly is defined as "spectrum of anomalies that involves the absence or hypoplasia of the radius, radial carpal bones, or thumb". It's found to ultimately be caused by genetics. During the ultrasound, the thumb or radius may not be present! In addition to an abnormal position of the hand... I don't think bowing is implied, but the length of the fetal arm may vary!

Doing research on abnormalities, honestly broke my heart & was crying for a good time. As sonographers, you don't really realize that we're the ones who must be vigilant in finding these abnormalities to advocate a healthy baby and safe delivery for the mom- to- be. As Lania and Allison covered, its important to understand normal structures of the fetal skeleton & ask the parents if there is any family history to be aware about! I need to get in the habit of asking this question before every OB scan.

Have a great week at clinicals c/o 2021!
Resources:
- https://radiologykey.com/radial-ray-deficiency/
- https://www.ajog.org/article/S0002-9378(19)31131-7/fulltext
Monica,
I loved your post, you always bring so much sincerity and compassion to the discussion! I mentioned in a posting earlier about the first time I observed an OB exam and the baby had skeletal dysplasia. Even though it was just a few short weeks ago I witnessed it ,I find myself thinking about it all the time. It broke my heart to know a young mother was going to raise a baby with a disability and myself and the technologist were the only ones in that moment that knew something wasn't right. I think that will be hardest part of our jobs is the heartache of recognizing disease and our patient is none the wiser. They may go about their day unsuspecting, but we know eventually they will get the results of our exams and be devasted. On the other hand that's why I love sonography because our attention detail won't necessarily prevent a disease, but it can change the way it's managed for our patients.
Getting back to the topic at hand (no pun intended) I wonder how common this anomaly is and if treatment options may be available?
Hi Chrishawna!
Duane Radial Ray Syndrome (DRRS) occurs 2 out of 10,000 babies. It's caused by a mutation in the SALL4 gene, this gene provide instructions for making the proteins for the development of the fetal tissues/ organs. The syndrome is inherited in a autosomal dominant manner. However, a de novo mutation may occur-- mutation occurring in the first time of a person with no family history of the condition develops. I have seen that there is corrective treatment once the baby is born. Although this syndrome has different severities! So it may take up to eye surgery, corrective heart surgery, hearing aids, and growth hormone therapy.
Thank you for your collective response. At my site, there is also a high risk pregnancy department-- so I typically only see healthy babies. It's great at getting exposure of what a normal fetal OB is. Whewwwww, I love hearing your stories and experiences at clinics, especially having Paris and Dr. Wilson there. Can't wait for FriYAY!
Hi Monica:)
I really like your post because during the audio lecture, this wasn't clicking for me right away but reading your post and seeing your pictures is really helping! I'm glad you chose this topic. I actually didn't know at first that this anomaly affected the thumb but thinking about it now, it makes total sense as to why it would. The anomaly image looks so off and I think I would be able to catch this while scanning! It's the very subtly abnormalities that I'm afraid to miss. This can apply to every exam though, not just OB. Missing something is incredible serious and I pray I never do once I'm in my career.
Hooola Hailey!
DRRS actually has different severities... I'm curious how many other abnormalities have different abnormalities! It's so much. Write this up, I feel like there's so much more to this-- my response above, to Chrishawna, implies more information about this syndrome. I hope that helps you out too!
Have a great week at clinicals!! (-:
Hi everyone,
I love this week's topic because it is such an interesting one and is a great way to learn more about and simultaneously lock in any abnormalities we may encounter while scanning OB.
While checking that baby's major bones such as femur, humerus, ribs, spine, and cranium are normal length, density and shape, we must remember to spend some time on hands and feet, to make sure the little piggies are formed and growing properly!

Normal fetal hands should show all 5 digits growing properly and of different lengths (the way normal fingers are), and just the simple motion seen of baby clenching and unclenching their fists can rule out so many abnormalities already.
One abnormality that I feel can be easily overlooked is "trident hands." Trident hand is a malformation of the hand that can be seen in utero, demarcated by short, stubby appearing fingers of even length, and a larger separation of the third and ring finger. This abnormality is typically related to achondroplasia, which would include a whole host of other possible skeletal dysplasias, and so if you were to see this as a possible diagnosis it would be good to double check all other measurements.


Just to really quickly go over achondroplasia-- it is a mutation in the FGFR3 (fibroblast growth factor gene 3) that causes abnormal cartilage formation, affecting the ossification of some bones. It is the most common cause of short limbed, or rhizomelic, dwarfism. Some other abnormalities we may see with this congenital disorder would include shortened and bowed femurs, frontal bossing, flattened nasal bridge, anterior flaring of ribs, and increased uptick in angle from lumbar spine to sacrum.
Here's a great article for more info:
https://radiopaedia.org/articles/achondroplasia?lang=us
Wow! I honestly think I could scan right by a fetal hand with this appearance and not even notice anything wrong at this point, which is scary! I see how the US does show the hands as kind of stalky and the fingers don't look normal after having it pointed out. This week's board has really alerted me to the little things I could easily be missing and why documenting every single part is so vital.
Hi Karen,
Awesome job on your posting and I love that you went the extra mile and included extra information on achondroplasia!! Hands and feet are one of the things that completely elude me when I am scanning OB. I think I am too focused on the big stuff like cranial anatomy, heart views, Biometry, and long bones that I hands/feet are swept under the rug. I am curious what the clinical significance of trident hands is, does baby still have the ability to use their hands normally or are there some limitations? At first glance they didn't necessarily look abnormal to me, but re-reading your post I now see the fingers are all about the same length and the increased distance between the 3rd and ring finger.
Hi Chrishawna!
Same here, this class has for sure made me more aware and cognizant of everything we are scanning. Hopefully, I will get to scan more OBs soon as I barely see any at my site at the moment! It must be exciting to be able to relate what you do at clinics to this class.
For trident hands, there is usually some limitation in the sense that they may not get full extension of their fingers, but it seems like this is mild compared to some of the other skeletal abnormalities we've been discussing in this post.
This article is long but I like searching key words and reading snippets about the different types of hand and foot abnormalities that it covers. It even has Marfans in there!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041879/
Thanks
-Karen
Hi Karen,
That's so cool that your article covers Marfans syndrome, what a throwback to Q1 LOL! Your posting has had me extra aware of fetal hands because at first glance I honestly didn't notice anything off in the images you shared. I am wondering if this might be easier to identify in the 3rd trimester as everything gets a little bigger on the baby and the move a whole lot less! Great Job!!
Hey Karen,
This was really informative! I was not aware of this anomaly. It makes sense this anomaly is related to achrondroplasia since the digits are not developing into their full size. Trident hands seem like it would be challenging to diagnose Sonographically. From the picture I looked up it seems as if we may have to look for fingers that seem abnormally separated.

Awesome post Karen!
Hi Karen!
I really like that you decided to talk about a hand anomaly! something so small can have some serious problem, although not life threatening, still serious none the less. I remember Dr. Wilson said we won't be sitting there counting the digits but an abnormality like this should not be missed, especially if we are paying close attention to all fetal parts as we should. I also appreciate you going over achondroplasia again, it didn't really stick with me after lecture. Double checking measurements is a great idea after finding an abnormality like this that affects the length of the bones directly. Good call!
Howdy Karen,
Which little piggy went to the market?
Sometimes people will see adults with trident hands and assume they're marking the Vulcan hand sign. This short video explains a little more about it. https://www.youtube.com/watch?v=hyVYH11cO_w
Please take a minute to watch if you can. It helps to humanize what we see with US!
Sarah
Hi Karen,
I did not know to look out for this! This shows how important it is for us to not only have good scanning skills but also be very knowledgeable about different abnormalities so we do not miss them. Have you learned any tips to scan the fetal hands at your site? I have issues trying to get a very clear picture and now I am worried I might have missed something like trident hands.
Hey Karen great pathology that you chose I feel like it would be difficult to spot this while doing a second trimester scan because the digits are already so small and sometimes the fist can be clenched are in the mouth of the fetus making it difficult to visualize. I believe I remember Dr. Wilson saying that you do not need to look or count of the digits so I’m wondering would it be a noticeable pathology for you to spot? have you seen this pathology in the clinics?
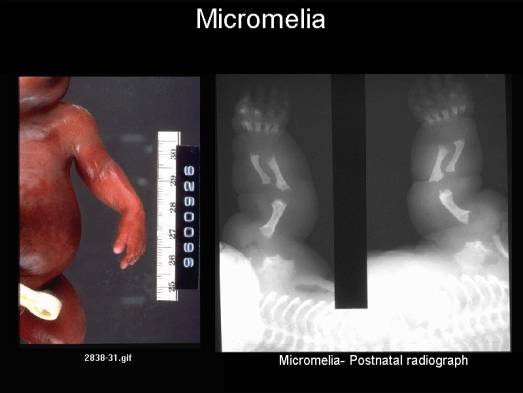
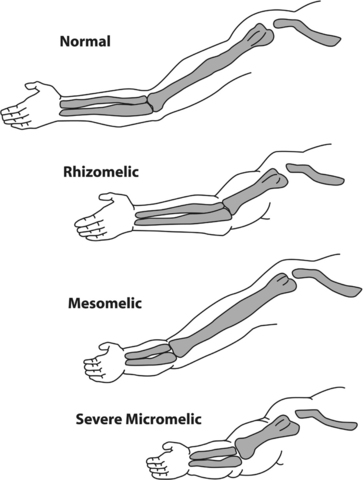
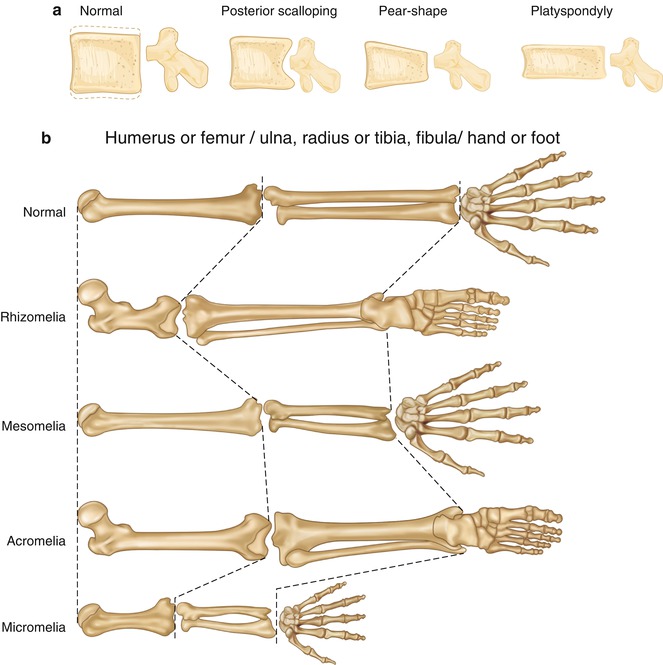
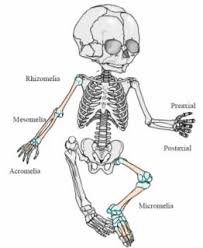
Micromelia occurs when the long bones shorten proximal and distally. (effects the entire limb)
Rhizomelia is when the proximal bones is shorter than the distal bones. (humerus and femur)
Mesomelia is when the shortening affects the distal bones most. (radius, ulna, tibia, or fibula)
Acromelia affects the hands and feet.
When there is limb shortening the femoral length cannot be used to measure gestational age.
The pictures below are super helpful in determining normal and abnormal skeletal appendages length. Normal could be determined because the humerus and ulna/radius are usually within good proportion to each other while acromelia for example might not have proportionate fingers.
This condition is usually inherited from the parents.
IMAGE OF A NORMAL FEMUR
IMAGE OF MICROMELIA

Hi Candee!!
You picked my favorite group of anomalies (I know that sounds weird) and some amazing pictures to match! This is one of the topics I spent a while looking at online after Dr. Wilson video lectures last week. I think I like it because I can clearly visualize what each type looks like and how they're different. This is another anomaly that I wonder how much genetics plays a role. If both parents were on the shorter side and what point do we classify this as normal for this baby or micromelic? I believe Dr. Wilson said that familial factors can begin to play a role later in the pregnancy, sometime during the 3rd trimester. Maybe if the patient comes for a 20 week scan and baby is below 2 standard deviations on their gestational age we would consider this?
Hi Candee,
Great job on your post, love the images that really explain the different types of "-melias" !!
It is good to note that fetal micromelia, like we went over in class, can be classified as mild or severe. Some may be related to other gross abnormalities that may render fetus incompatible with life, so this db also once again shows how important our jobs as sonographers are!
I found this article that includes an interesting case report, for anyone that is interested in a read! It's under the "full free text"
https://europepmc.org/article/med/32549900
Thanks,
-Karen
Hey Candee!
This is a great breakdown.
I saw that rhizomelia is common in achondroplasia. And that when rhizomelia and mesomelia aka micromelia are present there could be increased skin creases and skin folds due to the shortened bone length. This kind of correlates with the image you have!
Here is an image that corresponds with achondroplasia.

Howdy everyone!
During an OB scan we should see a normal fetus with 4 long limbs. The proximal parts will have 1 bone each and the distal parts will have 2 bones each. The first image shows normal fetal limbs.
Amelia is absence of one or more limbs (or shrunken/deformed according to WIki). This finding can be isolated or present with other abnormalities.
https://www.youtube.com/watch?v=lumXCYSuoqg This man has tetra Amelia Syndrome and is lacking all four limbs. ---- https://medlineplus.gov/genetics/condition/tetra-amelia-syndrome/#:~:text=Tetra%2Damelia%20syndrome%20is%20a,leg%20to%20develop%20before%20birth.)
WARNING: POSTMORTUM FETUS https://sonoworld.com/fetus/page.aspx?id=330
Sarah

Hi Sarah!
Amelia is such an interesting, yet sad anomaly. I'm curious about how the internal organs and systems would develop if they were missing multiple limbs. For example, if the fetus was missing both legs, I wonder how would the pelvis and organs would form?
Have you come across any statistics about if it is more common for fetuses to have upper limb or lower limb agenesis?
Here's an image of a baby with a missing arm.

Hi Sarah,
The video you linked was so fascinating, I would've loved to see the full episode and hear Szabolcs's life story. I was so amazed to see how he moved around with ease and didn't let his circumstances define him. The video cut off before we were really introduced to his adoptive parents, but from the clip of his mom in the kitchen I am under the impression she too is missing at least one limb. Since the fetus will have no long bones to measure for typical fetal biometry can you think of anything else that could be used as a parameter to estimate gestational age aside from BPD,HC,&AC?
Hi Sarah!
Great post, it made me dig more into amelia and what could cause it... apparently it may be linked with other congenital anomalies like oomphalocele and diaphragmatic hernias! And usually what causes this is exposure to teratogens, even Thalidomide, a cancer drug.
Radiopaedia even mentions that 60% end up dying postnatally depending on severity of amelia complications.
https://radiopaedia.org/articles/amelia?lang=us
Sad stuff...
-Karen
Happy Wednesday Everyone!!!
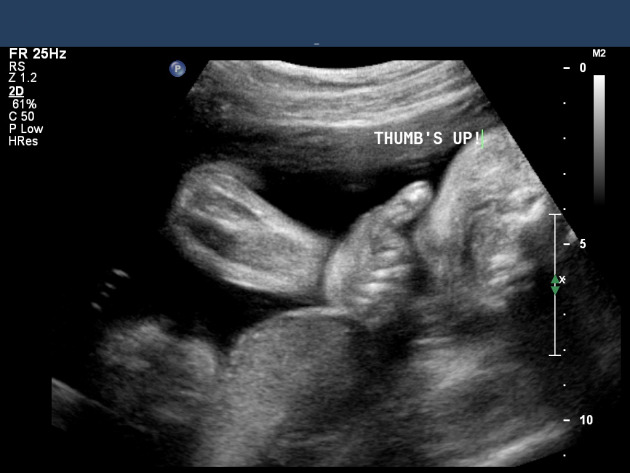
Hopefully everyone is having a great week and learning lots! Here's a neat picture I stumbled on that I thought was fitting for this weeks discussion :)
BTW, you are all doing fantastic on your responses, I can hardly keep up with all of you!!
Hey Everyone,
We're more than halfway through the week and I can't believe all of the postings you've shared!! We discussed on Monday some important questions a sonographer should ask their patients prior to the exam. Do you or your CI's have specific questions that are always asked, or if not, what would you ask a patient coming in for her 2nd trimester anatomical survey?

Great job this week Crishawna!
I really liked the list of questions Paris shared with us as an example. The techs at my site usually ask questions such as:
- How many times have you been pregnant?
- How many live births?
- Do you know what you're having? (gender)
- (If they don't, they usually ask them if they would like to know)
- How has your pregnancy been going?
Aside from these, I think it's also great to ask slightly more sensitive questions such as
- How were your previous pregnancies, did you have any complications?
- Do you have any family history of any anomalies/genetic defects?
I'm working on getting better asking relevant questions to all my patients before an exam, as well as explaining/narrating as Sue mentioned, so this is a really great question Crishawna!
Hi Zuly,
These questions are great!! One of the things I need to work on is asking my patients more questions before we begin, I always find once I start scanning a question or two I wish I would've asked. Sometimes I feel a little awkward in my delivery of the questions, I need to speak with confidence so patients feel they can trust me and will receive the best care! :)
Great job moderating this week! One thing techs always ask, and that I've started doing when I'm talking to a patient, is "Do you know what you're having?"
Just because we need to know if they don't know and want to keep it a surprise. Most of the time they already know because of the blood test, but sometimes they don't want to know so it's important to refrain from using pronouns.
So far I've only seen singletons, but I'm excited to see multiples!
Hi Leah,
I think this a great question to ask and from what I've seen so far it seems the majority of patients already know the gender from prior lab tests, but want to "double check" with a sonogram. I don't think patients realize the lab tests are much more accurate than ultrasound, but I do think it adds peace of mind when both results match!
Hey Chrishawna!
Great question for everyone!
My CI also asks the patient if they know what they're having and how their pregnancy has been for them. I've found that they don't ask about prior history regarding any anomalies in previous children or in family members. My CI does ask if its a first pregnancy or how many other children they have. I want to ask if I am allowed to ask that in clinical's. It's hard at times because you don't want to step over your CI, but you also want to try to perform what we're learning in this class. I do like how my CI narrates the exam to the patient. I try to do some narrating while scanning, but at times I need to really concentrate on getting images.
Hope your week in clinical's was great! Wonderful job moderating!
Hi Molly,
I totally understand what you mean about not over stepping. I noticed the questions that are asked are different depending on which technologist I am working with and I don't want to say the wrong thing or offend anyone if I ask any additional questions. I think once we start these exams on our own we may feel more comfortable asking questions, but it can be difficult if we are the ones back scanning. I also find when I am scanning OB I spend a lot of the time trying to talk myself through it and orient, hopefully one day soon I can multitask a little bit better!
Hi Chrishawana you’re doing a great job moderating this week and keeping everyone engaged unfortunately at my site we do not get a lot of second trimester OB or OB at all however I am sure the outpatient clinic does. But the small amount that we get by here my CI asks if the patient pregnancy has been going well or how it has been with their previous pregnancies. They also usually ask how many times they’ve been pregnant if they’ve lost any children previously and questions like that. I haven’t heard any of the techs that I follow ask the patient about a history of skeletal diseases or family history but I’m kind of curious about why they don’t. This class is definitely when me realize how important it is to ask your patient about family history and any information that would help you better scan.
I would ask you if your site asks any specific questions but I’m sure Dr. Wilson (OB GOD) covers all the bases!!!
Happy Friday Ladies!!
You have all worked so hard and shared such great information/resources! I will be wrapping up this discussion board tomorrow morning so be sure to get in your final postings soon and if you haven't already, check out the case study that Dr. Wilson shared on the main page of this discussion board, it is so fascinating!!