How is the location of the placenta determined within the uterus? Does this location remain constant or does the placenta move? Is there a bad location within the uterus for the placenta to implant? If there is, what makes this a bad spot, or not a good area to try and set up a foundation in?
Week Three Discussion Boards
The placenta plays an important role in the development of a fetus and sonography is a great tool to assess the location and size of the placenta. Its location typically depends on where the blastocyst implants within the uterus. As we learned previously, the trophoblast cells around the blastocyst are the precursors to the placenta and aid in its formation.
The placental location can move throughout a pregnancy, however it isn't technically moving on its own. Since the placenta is attached to the endometrium of the uterus, it will grow and shrink as the uterus does. This is why the placenta can sometimes be seen lower in the uterus during the first or second trimesters, and then it will be seen higher in the third trimester as the uterus grows in size.
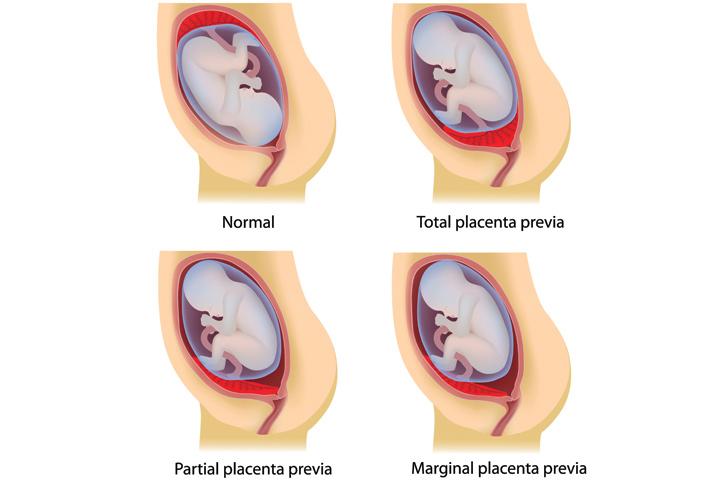
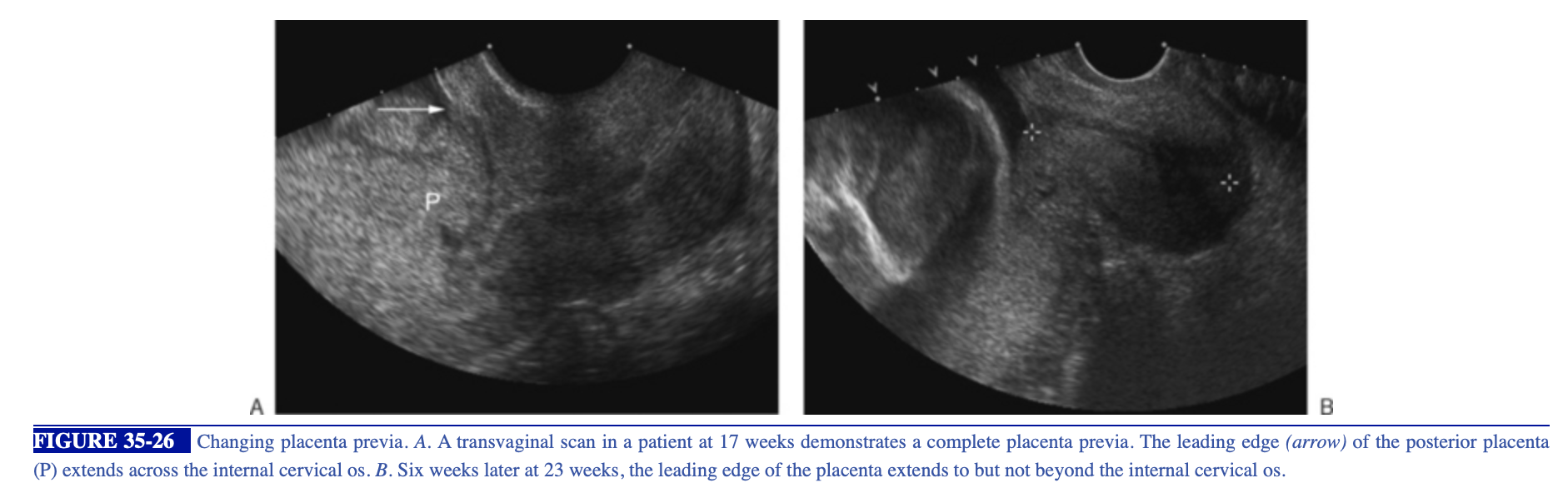
While to the fetus it doesn't really matter where the placenta implants, as long as there is one to provide it nutrients, the location definitely matters for the mother. A bad location for the placenta to implant would be right on top of the internal os of the cervix. This is called placenta previa. This is dangerous for the mother and she will likely need to undergo a C-section in order to deliver the baby, as there may be life threatening bleeding if she delivers vaginally.
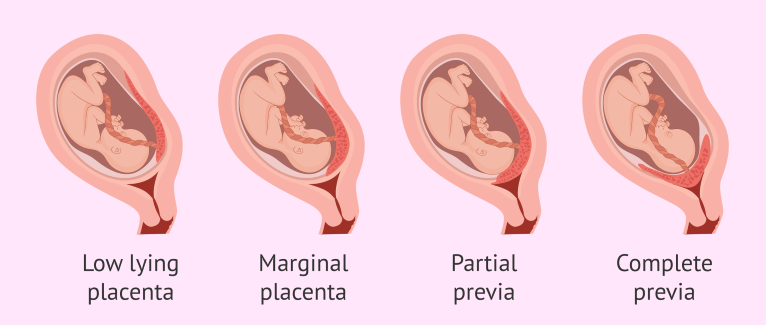
There are several types of placenta previa with complete or total being the most dangerous. Here is a diagram to help with visualization of the types of placenta previa!
Hey Brittney!
Great response! I love images you have attached as well. When I was reading an article it describe placenta previa as partial or complete. So it is nice to have additional terminology to add to it.
I also was thinking anterior placement of the placenta puts the mother at a higher risk for placental abruption. I understand it doesn't have direct cause on child birth, but still a thought. Do you think that an anterior placenta is a slight cause for concern? Or can possibly cause the mother to be even more cautious than usual?
Good morning, Nailah!
You bring up a great question and I was curious about anterior placental placement too! I did a little research and found a study which concluded that an anterior placenta is associated with an increased risk of conditions such as, placental abruption, intrauterine fetal death, and gestational diabetes. Here is the link to that study, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3935544/
I also remember reading on a different article how an anterior placenta can cause challenges for the sonographer and clinician. If the placenta is right in front of the fetus this can definitely make imaging harder! The article also explained how an anterior placenta can make procedures, such as an amniocentesis, more difficult as well as there are additional layers to penetrate and watch out for.
An anterior placenta can also limit the ability of the mother to feel fetal movements, and the clinician's ability to hear a heartbeat. I'm sure this can cause concern if they do not know it is because of the placental location.
An anterior placenta definitely seems to have its risks, however with proper care and monitoring a healthy pregnancy is possible.
Hey Brittney!
Thank you for sharing that research, all super interesting information. How an anterior placenta can affect imaging makes sense. Through my experience at clinicals thus far, I am becoming aware that fetal positioning is so important for optimal imaging . For example, for optimal assessment of the fetal outflow track, it is best that the fetus is lying on its spine belly upward.
I also was unaware that an anterior placenta can cause fetal abnormalities as well. All very useful information, Thank you !
Location of the placenta is determined by where the blastocyst implants into the endometrium 7-9 days after ovulation and fertilization. After decidualization occurs, the decidua basalis becomes the maternal contribution to the placenta. This is referred to as the basal plate. The chorionic villi from the embryo embed into the endometrium as the fetal side of the placenta. This chorionic plate is a fused layer of amnion and chorion with blood vessels. Below is an image I found that really helped me understand what the interface of the placenta looks like.
The placenta functions as the site for all nutrient and gaseous exchange between the mother and the fetus (however the two blood supplies never actually mix). It also serves as a protective layer with metabolic functions and helps maintain the pregnancy by producing hCG, estrogen, and progesterone after the corpus luteum regresses after 10 weeks.
While the placenta and uterus will grow, the location of the placenta is constant due to implantation. It's relative position may change as the uterus grows around it throughout the pregnancy. While there are many lovely spots for the embryo to implant within the uterus, there are some spots that can create real problems... like placenta previa.
Placenta previa occurs when the placenta's location obstructs the cervical canal at the internal cervical os. This usually presents with second trimester painless vaginal bleeding, and there are varying degrees (from approaching the cervical os to completely covering it). It also requires a Cesarean section for delivery.

Hey there Leah!
Great response, it was very informative. I like how you italicized relative because it removes the assumption for beginners learning embryology that placenta is like detached and just moving around the uterus as the fetus grows.
I am still trying to my head wrapped around this whole maternal and fetal blood "do not mix" from the lecture. Would you say the process is comparable to gas exchange in the capillaries ?
The location of the placenta is determined by where the blastocyst implants in the uterus. I also learned that it’s hypothesized that the placenta may implant in the lower uterine segment if the upper endometrium is not well vascularized because of damage from a previous C-section, abortion (induced or spontaneous), uterine surgery, and multiparity. https://www.youtube.com/watch?v=eMm6nCiK_no
Since the placenta is attached to the uterus, as the uterus grows up superiorly away from the cervix, the placenta will “move” up and away from the cervix with it. However it’s important to understand the placenta doesn’t actually “move” all over the place, it’s “not on legs” as Dr. Wilson explained.
Placenta previa is when the placenta is located in the lower uterine segment, on top of/covering the internal cervical os. These mothers often need to have a C-section, and are sometimes put on bed rest if they are experiencing painless vaginal bleeding. So this would be a bad location for the placenta. There’s variants of placenta previa which include low lying, partial/marginal, total/complete and asymmetric complete.
I came across this image and thought it might be considered “partial/marginal” placenta previa, although I'm not 100% sure!
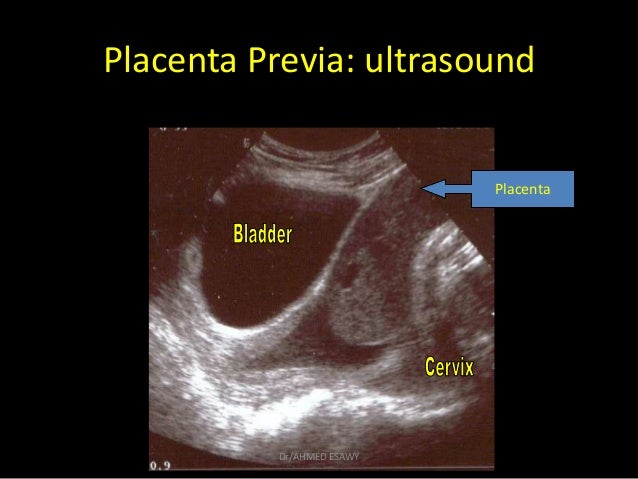
That's an interesting hypothesis Zuly although I don't completely understand. Are you saying that damage of the uterus could effect where implantation takes place? I wonder if a blastocysts could implant at the same spot as a previous implantation? (Dumb random thought) I like you picture as well I would probably agree and say that its partial obstruction of the cervical canal. Is the fluid above it form the gestational sac?
Hi Candee!
I think it means that if there is some type of damage to the uterus, there's possibly not enough of a thick endometrium able to be built up in that spot and therefore it wouldn't lend itself to be an implantation site? I love the thought you had about if the same spot can be an implantation site twice! Maybe that spot would be "worn out" after the first time so it wouldn't be as vascularized, so the blastocyst couldn't implant there. I'm not sure I'm just hypothesizing but it got me thinking! Also Paris commented below on the photo, she mentioned it's a bit confusing so she posted a more classic appearance one that should help!
Hi Zuly !
Thank you for knowledge drop! I didn't know poorly vascularized areas in the fundus of the uterus increase the likelihood that the placenta will cover the cervix. I wonder if it because like the examples in the video provided in cases of scarring and multiple pregnancies cause the placenta to favor a side? But would this also suggest the blastocyst favors to implant in an area of high vascularity? I also wonder if it this idea can have the reverse effect? Like a poorly vascularized lower uterine segment causing the blastocyst to implant higher?
I would also like to think the image represents a partial placenta previa. This article I read leads me to think so.
https://parenting.firstcry.com/articles/common-placenta-positions-an-overview/
Hi Zuly! That is an interesting point about the lack of vascularization post-surgery, post-trauma, and post-pregnancy. It does make sense to me since the area of incision or trauma would likely develop scar tissue and thus be less vascular. I read this article that did an analysis on patients who delivered via C-section and the subset of cases that were indicated by placenta previa. The study found patients with previously scarred uteruses who delivered via C-section because of placenta previa accounted for ~11% of the C-sections compared to patients with non-scarred uteruses at ~6% of the C-sections.
The placenta is really important because it helps maintain the pregnancy such as maintaining homeostasis, transfer of nutrients and gas exchange. The placenta grows from where the trophoblast decides to implant in the uterus. The decider basalis is the maternal contribution of the placenta while the chorion is the fetal contribution of the placenta. It can be located anywhere in the uterus (Ant, Post, fundal, R lat, L lat, lower uterine seg). When the placenta is implanted on the cervix, placenta previa might happen which occurs in 1/200 deliveries. (Not the best place for implantation) There are three types of previa low lying, partial, or total. Placenta previa is when the placenta is located on the internal os and might result in C section. I also remember hearing about another type of previa but can't recall which one it is.

Hello again Candee!
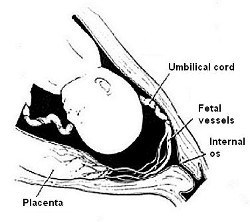
I believe the other previa condition that you mentioned is Vasa Previa!
This is when the fetal blood vessels are really close to the internal os of the cervix, but still in the amniotic membrane. These vessels can become compressed by the fetus during birth and this can lead to decelerations of the fetal heart. There is also a high risk of bleeding if the mother delivers vaginally. A C-section is typically done in these cases.
Here are some images to help with visualization! Also Radiopaedia had some great information on this :)
https://radiopaedia.org/articles/vasa-praevia-1?lang=us

Thank you for telling me Britt! I could not figure it out. Would this condition be worse than the placenta previa?
Hi Candee!
I'm not sure if one of these conditions can be considered worse than another, as they can both result in dangerous hemorrhage.
As I was reading about Vasa previa it noted that a high percentage of mothers with this condition during their pregnancy also suffered from placenta previa with that same pregnancy. Perhaps the two are often connected?
They both seem to have decent prognoses as long as the fetus is monitored for any distress and the mother undergoes a C-section to avoid the hemorrhage that is likely with a vaginal delivery.
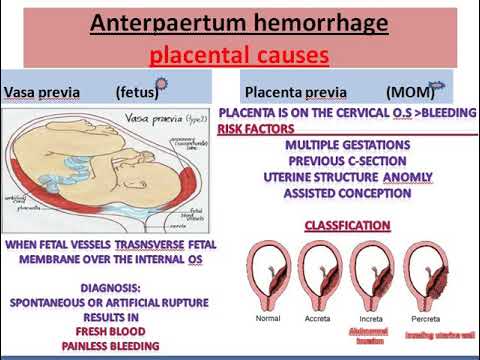
I found this nice little graphic which helps with remembering the differences between the two conditions!
Hey Candee,
Nice work! I was reading an article and it was describing the second image as partial placenta previa and the other as a complete placenta previa. Thank you for introducing me to the knew knowledge. There are so many terms that represent the same thing, so the more familiar we all can be with them the better. I am curious if a mother diagnosed placenta previa causes stress to the fetus in anyway? What do you think?
Hm I could imagine that any news about blockage of the cervix could be scary for a Mom but I think it might not be that bad because the placenta could continue to grow through the 3rd trimester. Still really scary. What has been the scariest thing you have seen in clinicals
Hey Candee girl,
Indeed it does seem very natural for the mom to be nervous. My question was regarding the fetus and if placenta previa caused any stress to the fetus? I’m sorry if that was confusing.
I think so far in my clinical experience a woman with fibroids throughout her uterus and complex cyst in the ovaries, has been the most memorable. It worried me about some form of uterine or ovarian cancer, maybe even both? The uterus was nearly unrecognizable. My heart definitely goes out to her.
The mother would have to be pretty significantly stressed, but typically previas are very manageable. As you both mentioned, the likelihood of the placenta moving away from the internal os is high. However, if it doesn't, mom is typically put on bedrest and has a scheduled c-section for her delivery. You'll see throughout this class, MUCH crazier things happen.
Hi Candee,
I like the image you included! The other types of previa are low lying and partial/Marginal. partial will be partially covering the internal os but won't be attached on both sides.
https://www.mayoclinic.org/diseases-conditions/placenta-previa/diagnosis-treatment/drc-20352773
I found this website and it explains how there "treat" the patient based on bleeding levels.
What do you think would happen if a baby had placenta previa but they tried to do a vaginal birth?
Hi Candee,
I love the picture you included in your response. It really helps lock in the concepts for a visual learner like myself. I think that the other previa you are talking about is marginal previa, in which the placenta begins to grow at the bottom of the uterus and pushes against the cervix without covering it.
https://www.healthline.com/health/placenta-previa#types

The placenta is a huge part in the development of a baby because it allows for nutrients to be exchanged for proper fetal development along with respiratory and excretory assistance. The placenta becomes attached to the uterine wall via the trophoblasts which determines where it’ll be located. The placenta is implanted to the uterine wall and can be located at any place within the uterus, but it cannot move all over. The placenta is normally located within the area of the fundal region of the uterus, but some can implant elsewhere and cause some issues. A location that can be worrisome is within the lower uterine segment blocking the cervix, which is known as placenta previa. This location is the worst one possible for implantation. The placenta can either partially or fully block the internal os of the cervix. It seems that if this were to occur early on in pregnancy then it wouldn’t be a big deal because as the baby grows the uterus also grows (stretches out) and the placenta is dragged (moved upward and out of the way of the cervix) with it. With this occurrence, a baby could need to be delivered via a cesarean section if it were to persist into the third trimester.
Here's a video I found helpful explaining placenta previa and the different times within pregnancy this diagnosis can become a concern:
Hi Molly!
Thank you so much for sharing that video, that was the best explanation of placenta previa I have seen! The presenter did a great job breaking down all of the different components that can lead to a previa and taught me some new vocabulary! I kept hearing the word "antepartum" but had no clue what that meant, but according to the video it refers to 20 weeks or greater of the pregnancy. I also liked that she mentioned the different causes, some of which I was familiar with, and others were completely new. She mentions that mulitple gestattions, hx prior placental previas, and even hx uterine surgery.
Here's a cool article that shows placenta previa across a range of modaliities, I thought you might like this with your background in MRI :)
https://pubs.rsna.org/doi/full/10.1148/rg.295085242
Hey Ms. Molly,
Thank you for sharing this video! Khan Academy is a great resource to use the when we need a little more help creating a visual. I think it is interesting the placenta usually favors the fundus region, I read that too. Do you think it is because as the baby grows it just tends to cause the placenta to migrate upward? I'm curious if how the baby grow affects where the placenta migrates.
Hi Nailah and Chrishawna,
I’m glad you both found the video useful. Khan academy is definitely great at explaining! I agree with you Nailah about the placenta tends to migrate upwards with growth! My CI also emphasized how the fundal region is the best possible location for the placenta to implant at and if placenta previa is seen early on then it most likely will move upward towards the Fundus on its own because as the baby is growing, it’s pushing the placenta up and out of the way. There was a case today where a second trimester OB case was being scanned and the cervix was being imaged TV. My CI did a sweep and in one view it looked like the placenta was starting to block the internal os. Since the pregnancy was still early into her second trimester, my CI documented and said they would keep monitoring her case and scan her to see the progression or hopefully lack of progression.
Thank you Chrishawna for sharing the article on other modalities imaging placenta previa cases. That was very interesting to see. Also awesome to view the MRI images too! I know MRI rarely ever imagesOB cases at least not at my work, but I do wonder how often other facilities do MRI‘s for placenta previa studies.
Howdy Molly,
Khan Academy is great! I try to keep reminding myself that the placenta has two parts: mom's (decidua basalis) and fetus' (frondosum). So here I am reminding everyone again!
I answered "no" when asked if the placenta moves but I think you're right! We can technically answer yes. Although, if it were to truly move both mom and baby would be in trouble. I think the blastocyst would have to implant quite near the cervix for previa to occur (since the uterine growth tends to move it superiorly).
A fun side note about placentas I learned in clinic today: placentas tend to get old and end up with calcifications toward the end of pregnancy. This is totally normal!
Sarah
The placenta holds the connection between the mother and the fetus. The location of the placenta be anywhere within the uterus. However the location of the placenta is determined by the blastocyst. This occurs in the endometrium of the uterus about 8 days after ovulation.
The location of the placenta remain constant. This organ continues to move throughout the pregnancy with the help of another organ. As the placenta is tethered to the endometrium of the uterus, it will expand and/or condense at the same pace. It's rewarding to find that mainly ultrasound is used to determine the location of the placenta.
The internal cervical os, "door way from the uterus to the birth canal", is the worst location within the uterus for the placenta to implant. Placenta previa is when the placenta is placed from the fetus to the birth canal. This makes the worst location because it is covering the cervix, leading to an increased chance of a cesarean delivery (= long recovery time, vaginal bleeding).
I find it interesting that there is a saying "If a pregnant mother has a low belly bump, it's going to be a boy OR if the belly bump is high, it's going to be a girl". All while it is just the placement of the placenta! ...However I did guess both of my cousins' baby gender right by this saying.

Hey Monica, Britt also helped me discover vasa previa which I believe is another form of obstruction. This condition will be when there are blood vessels blocking the cervical canal. That's so funny that you added the fact about baby bumps because we also have that superstition in my family. Maybe it's true that boy zygotes like to implant lower in the uterus compared to males. I wonder if that's a thing. I tried researching but couldn't find anything LOL!
Hey Monica,
I love how you included the reward of sonographers being honored with role of assessing placental location. Such a dope perspective!
Also when you say other organ in the second paragraph what do you mean? The baby?
Pregnancy superstitions crack me up too! What is funny is I was taught the exact opposite; when the baby is round like a basketball and sits up it's a boy and then when the baby hangs low it is a girl. Too funny!
Hi Monica,
I love how well you explained everything! Also that superstition... I never fail to hear it when I see someone's baby bump!! You're right, it could all just be where they implanted!
Today at my site I scanned another 5wk gestational sac (this time with yolk sac!) and it was implanted more on the left side of the uterus. As my instructor and I examined the ovaries, wouldn't you know it?? The corpus luteal cyst was on the left side. I wonder if the ovaries make it more likely for implantation to happen on the same side as where the egg was released, or if it really is just totally random.
Karen
The location of the placenta is determined by the location of implantation by the blastocyst. We hope the placenta will grow within the uterine fundus but unfortunately it's all up to chance. The location of the placenta does not exactly change, but rather be shifted as the uterus grows.
The worst location for the placenta to “set up camp” so to speak, would be near or covering the internal cervical os. Depending on the severity of coverage we can categorize the placenta location. If there is complete coverage of the internal cervical os we call it complete placenta previa. If only a portion of the os is concealed it is a partial (marginal) previa. If the placenta is out of the uterine fundus and near the lower uterine segment within two centimeters of the internal os, we dub that a low-lying placenta.
A placenta that is not implanted in or near the uterine fundus, run the risk of having a c-section delivery. In the event of a previa a c-section is unavoidable given it is blocking the fetal entrance to the birth canal. This another example of why accurate measurements are essential in all areas of sonography. Being off by even a centimeter could mean the difference between a normal vaginal birth or major surgery for mom.
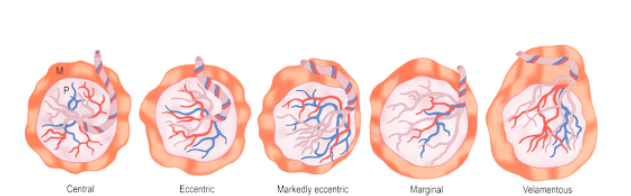
I have included a photo of the different areas of insertion of the umbilical cord into the placenta. Its just one more area regarding the placenta that we need to check during our scans!
Hey Ms. Chrishawna!
Great response! I like how you highlighted the importance of dedicated patient care because it is sooooo true! The slightest change in measurements can save a life. Also I enjoyed the images of umbilical cord insertion. Is important to stay open because anatomy does vary from patient to patient. Also I have been seeing my CI use color to asses perfusion to the fetus. I know we all were initially taught not to put color on the baby, but at the 20 week fetal ULS there a few instances in which color would be used. Additional examples include: kidney's, umbilical arteries, and placenta. Just a friendly reminder NEVER put color on the heart.
Hi Nailah!!
So glad you shared your clinical experiences, I love getting the inside scoop!! It's funny you mention the use of color Doppler during the 20 week anatomy scan, since that is what I am presenting next week. I have noticed CD being used quite a bit in my research so it seems like there is definitely a time and a place for it to be used. If you're interested in some additional resources to use related to color Doppler in obstetrics scans, I have attached a great resource below! It's really long and touches on a lot of physics concepts, but even if you can use it for images I highly recommend it! The great pictures start around the 9 or 10th page and go from there!
https://fetalmedicine.org/var/uploads/Doppler-in-Obstetrics.pdf
You are totally right Chrishawna! We must take the time and care necessary to help set up good patient management for mom. As Dr. Wilson mentioned in the lecture, we should evaluate a borderline low lying placenta pre and post void to see the true placental location relative to the cervix. An over distended bladder can push the placenta closer to the cervix.
This website, RadiologyKey, describes a few more scenarios that can cause a false flag for placenta previa.
Here is one scenario that Radiology Key describes. The top image shows a contraction of the myometrium (**) mimicking the cervix and placenta previa. The bottom image shows the uterus after the contraction.
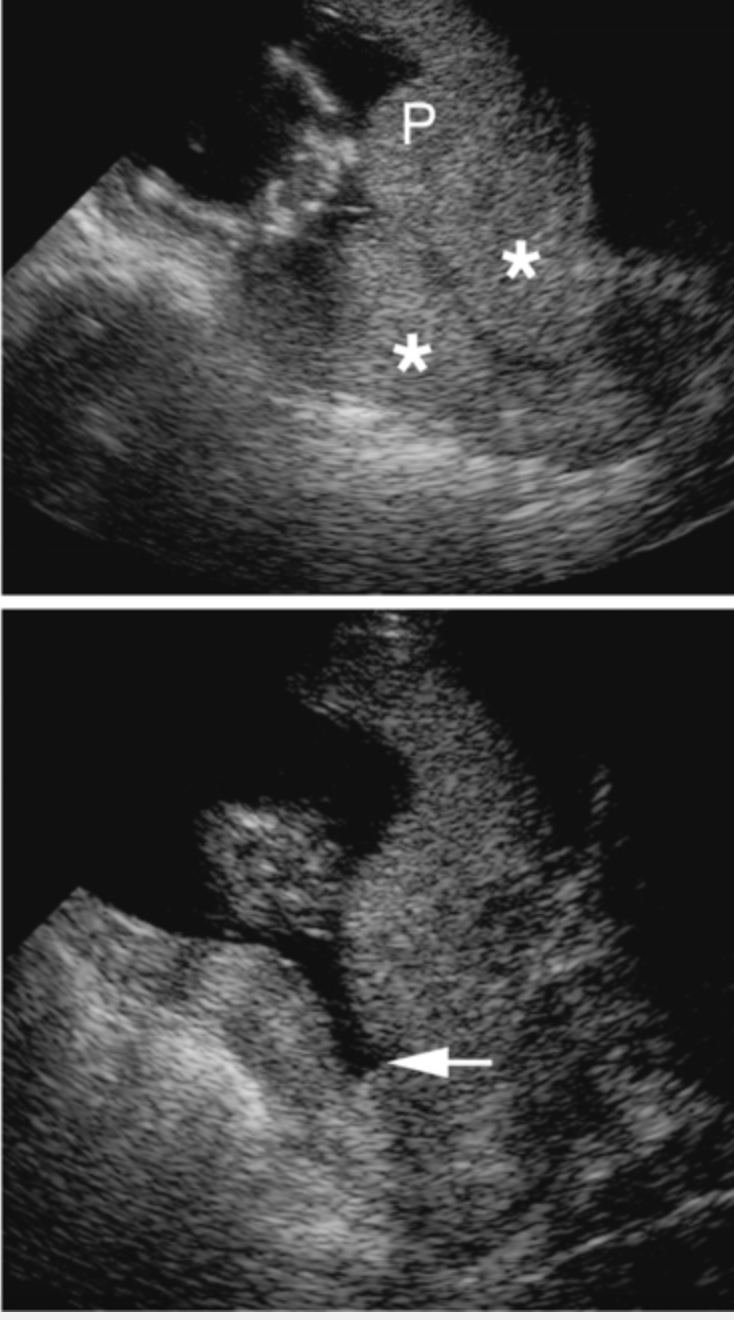
Hi Chrishawna!
Great answer and picture! I literally saw a placenta previa today in clinical and it just made me that much more aware of how important it is that we scan the placenta and cervix. I also learned that the mother could be having a contraction that could falsely make it look like placenta previa, so if you see possible placenta previa in the beginning go the exam, check again towards the end to see if it is true previa or possibly just a contraction.
This is huge! Thank you for mentioning this. As sonographer we definitely look at, not only where the umbilical cord enters baby, but also where it enters the placenta. There are several pathologies around this concept. Which area of insertion is considered normal?
Hi Paris!
I remember Dr Wilson saying we want the umbilical cord to attach centrally to the placenta, but there are two variants Battledore and Velamentous insertions that can occur! I found a cool article with some great images of umbilical cord insertion: https://pubs.rsna.org/doi/full/10.1148/rg.341125127
Just re-enforces how important our job is as sonographers to be thorough with every exam!
Hey Chrishawna,
Thanks for the image of the cord location. I am having a bit of trouble understanding the different variations. I did find that velamentous cord insertion is where the cord inserts on the edge of the placenta along the chorioamniotic membranes. This makes the blood vessels unprotected as they leave the placenta until they reach the umbilical cord where they are protected. Here is an image I thought was representative of the unprotected cords. It also highlights vasa previa which is where those vessels can get trapped making them at risk for rupture.

The location of the placenta is determined by wherever in the uterus the blastocyst attaches and implants into the endometrium. The placenta is made up of three parts. The first is the maternal side known as the basal plate and the second is the intervillious space where maternal fetal exchange occurs and lastly,the fetal side known as the chorionic plate. The location of implantation is where the placenta forms and will remain constant for the entire pregnancy. However, as the uterus grows the placenta will move along with the growth yet still be attached at the same spot. A suboptimal location for the placenta would be close to the cervix or in the lower uterine segment. This is a suboptimal location for the placenta to be in because it can cause placenta previa. This is when the placenta covers the internal os of the cervix. Essentially the opening to the birth canal when the baby is ready to be delivered. When the placenta is attached at the lower uterine segment or the cervix and the uterus grows this could cause a disruption in blood vessels and the mother may present with bleeding. For the mother this could be troublesome because of the blood that is lost and for the fetus this could cause hypoxia and preterm delivery. There are 3 categories of a low lying placenta. The first is low lying which is when the placenta is within 2cm of the internal cervical os. The second is partial or marginal placenta previa which is where the end of the placenta is covering the cervix. Lastly, a total or complete previa is when the placenta is completely covering the cervical os.
Here is a great video on placenta previa!
https://www.dailymotion.com/video/x653jw2
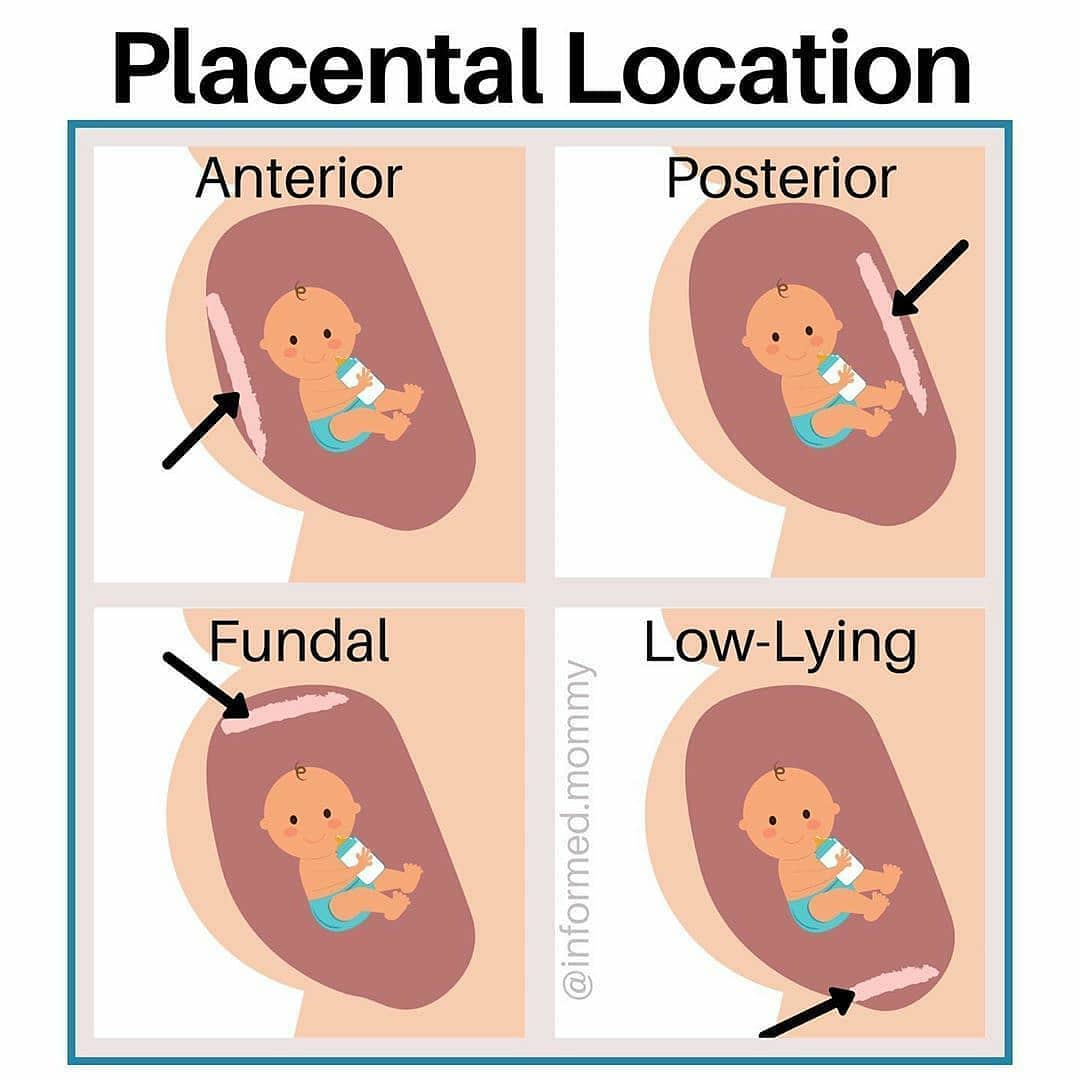
Also I thought this was cool for positions the placenta can present in the uterus!
The five simulated placenta positions (from left to right: anterior, superior, posterior, lateral left and lateral right).Hey Allison!
I really liked the visual you provided of possibilities the placenta can be located. As a visual learner that helps me a lot! Thank you!
Watching the video you posted made curious if the hypoxia, on the fetal end of placenta previa, was because in the cephalic position the head is essentially hindering perfusion of oxygen between mom and fetus? What do you think?
Hey Nailah,
I think hypoxia can occur with placenta previa because when the lower uterine segment grows and the placenta is covering the cervix bleeding can occur. With excessive bleeding the baby wouldn't be getting enough oxygen from the placenta because all of the blood is draining out instead of to the fetus.
Hi Allison,
We had similar answers! I really like your image you included, it's different from everything I've seen! Do you think theres any treatment for placenta previa?
Hey Hailey,
I think placenta previa is something that for sure needs to be tracked.I have read that if major bleeding does occur the mother can have transfusions to keep blood volume. However, if there is minor bleeding bedrest is usually the treatment along with check ups. I know a cesarian is most likely to be the birth plan. With a complete placenta previa you wouldn't want to have the placenta detach from the mother and be delivered before the baby. This can cause hypoxia where the baby would still be in the womb and be deprived of oxygen.
Hi Allison!
I loved how in depth you went about the three categories of low lying placenta. I kind of glossed over it as a whole "close to cervix" placental location but from what you wrote, you can really tell that minute differences in location can really matter!
I also love the visual you used. It's crazy to see how much the uterus balloons up in relation to mother's body, when the uterus generally starts at only about the size of a fist!
Thanks,
Karen
Hi Allison!
Thank you for including the photo, it helped me wrap by head around the different placenta positions, since it is a bit confusing with all the variations. The way you explained the reason for possible bleeding with a placenta attached to the lower uterine segment made sense to me because I was having a a little trouble understanding it. But it makes sense that it could disrupt the blood vessels as the uterus continues to grow. I liked this image because it clearly labels everything and it helps fuse together the diagrams and ultrasound images!
The placenta is a maternal fetal organ; meaning it needs some of mom and baby to preform all its amazing functions. Once the blastocyst implants itself into the uterus the chorionic villi (fetus) invade the decidua basalis (mom) to create this exchange of nutrients, or the placenta. The implantation site would be the location the placenta begins its development. The placenta’s location is not definite though. In early pregnancy it is typical for the placenta to lie low in the uterus. In later stages of fetal development “placental migration” occurs, in which the placenta will move towards the fundus, lateral, or posterior surfaces of the uterus. Placental locations in the uterus include: posterior, anterior, fundal, lateral, and placental previa. Ultrasound is used to accurately assess the placental location.
Proper assessment of the uterus is very important because expecting mothers are at risk for placenta previa, i.e. a low placenta that blocks the cervical canal; which can cause death to the mother and fetus during labor. Placenta previa can be considered partial or complete.
An additional risk a mother faces with placental development is when the placenta lies in the anterior portion of the uterus. An anterior placenta places the mother at a higher risk for placental abruption. Placenta abruption is caused when direct trauma occurs to the mother’s abdomen, such as a motor vehicle collision.
Here are two articles I read that help explains possible placenta locations and risks associated with them:
https://parenting.firstcry.com/articles/common-placenta-positions-an-overview/
Hi Nailah!
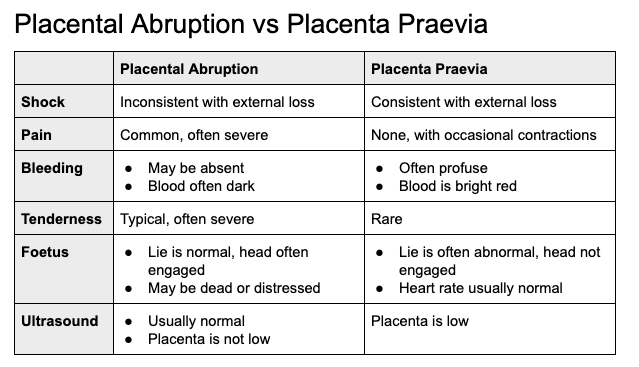
You bring up another dangerous condition; placental abruption. While we haven't discussed this in lecture yet, I found this nice little graphic which explains some of the differences between placenta previa and placental abruption. They can both present with vaginal bleeding, however there are some big differences to look out for.
For example, with placenta previa the bleeding is typically painless and the blood is a bright red color. With placental abruption, there is pain with the bleeding and the blood is a dark red color. These may be important signs to look out for on a patient's chart so we know what we will be seeing when we scan!
Hope you had a good day at clinicals :)
The location of the placenta is determined by where the blastocyst implants. The trophoblasts (chorion) of the blastocyst are the fetal component of the placenta and the decidua basalis is the maternal component of the placenta. The placenta does not move relative to the implantation site, but the placenta does move (usually ascends) with the uterus as the uterus grows.
There are unfavorable positions for the placenta to implant on or near the cervix. The positions are unfavorable because they can block the birth canal and/or cause severe hemorrhaging during birth, putting the mother and baby at risk. The most unfavorable place for the placenta to implant is directly on top of the internal os of the cervix, covering it completely. This is called total or complete placenta previa. Partial placenta previa is when the placenta partially covers the internal os. Marginal placenta previa is when the placenta is abutting the internal os, but not covering it. Low lying placenta is when the placenta lies within 2 cm of the internal os. These classifications are all associated with painless bleeding in the second half of pregnancy as the uterine lining thins to prepare for delivery.
Once diagnosed with a low lying placenta or one of the classifications of placenta previa, the cervical length will be routinely monitored via ultrasound to determine if vaginal birth should be ruled out in favor of a Cesarean section. This video about placenta previa states that 10% of low-lying placentas and placenta previa patients remain in the risky category throughout the pregnancy. I would be interested to know if anyone else found a similar statistic!
Hi Alexis!
Thank you for sharing that video you posted. I honestly didn't know 90 percent of the time placenta previa resolves in the third trimester. I guess I assumed it remained throughout pregnancy if it was present at the 20 wk ULS. This article does not necessarily say 10 percent but it does essentially state that the percentage of placenta previa cases significantly decrease in the third trimester.
https://www.parents.com/pregnancy/complications/health-and-safety-issues/all-about-placenta-previa/
Hi Alexis!!
It's so cool how the placenta moves along with the uterus. I found that the the location of the placenta can be sonographically imaged inaccurately if or while the mother is having contractions! The contractions can make it look like the placenta is laying low, near the cervix. I wanted to comment on yours, because I noticed that you listed all of the positions of the placenta ( super helpful btw ) and wanted to make note on how we should always be aware and ask the mother questions to make an accurate diagnosis.
Thank you for sharing!
The placenta has two sides: maternal which attaches to the deicidua basalis and the fetal side. In early pregnancy, the placenta takes up the majority of the uterus but as pregnancy weeks increase and the uterus size increases along with it, the placenta location will change. The maximum thickness of a placenta during pregnancy is 5 cm and anything about that would be worrisome. The placenta can be located anywhere in the uterus but our main goal with sonography is to see if the placenta is partially or completely covering the cervix. I actually found the cervix on a pregnant patient last week at my site and measured from the internal os to the tip of the placenta. A placenta that is low lying is implanted in the lower segment of the cervix and is seen if it is within 2cm of internal os. The placenta can also be partially covering the internal os and a complete previa is when the placenta is entirely covering the internal os. Placenta previa will most often lead to bright red bleeding and result in a C-section (https://www.mayoclinic.org/diseases-conditions/placenta-previa/symptoms-causes/syc-20352768). A marginal previa means that depending on how the uterus grows, most likely the placenta will move away from the cervix.
Hey Raminita,
I really appreciate the visualize you provided, visuals are always so helpful. I like how your example provides a reminder that placenta previa can occur whether the fetus is breached or vertex. Congrats on finding the cervix too! That's amazing!!! I know it is still all knew for us, but do you have any tips on locating the cervical canal in pregnant women?
Hey Nailah,
Great question! I might not have the best tips yet but I know that at first I was having an issue getting a good view. I kept trying to push straight down but with a baby in the way it's kind of heard :P. So what the tech that taught me did is have me come from the left of the patient's belly and slide with force behind the belly to get a good window to the cervix. Hopefully that makes sense but I can show it better in class. :)
Hi Raman! That's awesome you got to see what we're learning in class in real life!
Regarding the uterus growing and hopefully taking the placenta with it away from the cervix, I found the below image on RadiologyKey. It shows how the placenta went from being a complete placenta previa to marginal placenta previa over 6 weeks. This shows how follow up with these patients is important!
It is interesting that you mentioned that Alexis because today there was a case today where originally the placenta was only about 1.17cm away from the cervix and after we had the patient use the restroom, the placenta moved and was 3cm away from the cervix. The tech was telling me that if the placenta is less than 1cm from the cervix then we must do an endovag to confirm previa. I think these little tips show how much we need to use our critical thinking skills to better assess the patient.
I love these images!! Even aside from our OB simulations, I have been having a hard time identifying the cervix in the TV gyn lectures too because I just don't really see where the "cut-off" of cervix to uterus usually is. All these placenta previa pictures have actually really helped me though, since there is such a clear border of placenta to cervix! Who would think that abnormal sonographic signs would help me understand normal signs too!
THANK YOU for talking about the thickness of the placenta! As a student, I had a case where I noticed the placenta looked abnormally thin. The placenta was measuring only 1cm thick and during the exam, the patient was telling me she had fainted twice since becoming pregnant, but no one could tell her why. At the end of the exam I told the tech I was working with that I thought there was something wrong with the placenta. She assured me that the thickness of the placenta didn't really matter and that it could vary... I still didn't feel right. I asked several other techs and they all said something similar. THANKFULLY Michelle works at the site I was at so I was able to ask her. She agreed with me that something wasn't right and was able to call the reading physician to make a note of the finding.
This was something that maybe wasn't having too much of an impact at the moment, but could have put mom and baby at risk down the line. This is one of those times when you realize that it is SO important to look and everything even when it's easy to get complacent.
Thanks Raman!
Oh God, that is terrifying! I am so glad that you followed your tuition and the tech believed in your great skills as well. That is one of my biggest fears is missing something so even now I annoy my CIs by asking them so many questions so that hopefully I won't miss anything when I work on my own. Thank you :)
Wherever the blastocysts implants into the endometrium, determines where the placenta will be. The location moves as the uterus grows, it doesn't just move around on it's own because it's attached to the uterus, but as the uterus grows as the pregnancy grows, the placenta will move with it.
Depending on where the blastocyst implants, there can be a not so great location for the placenta. In this week lecture we learned about the different types of placenta previa: Low lying is when the lower segment is within 2cm of internal cervical os. This isn't too worrisome but should definitely be monitored. Partial or Marginal previa is when the internal cervical os is partially covered but not attached on all sides, this needs to be monitored closely because it has the potential to become full previa, which is when the cervical os it completely covered by placenta. In earlier terms with placenta previa, it will be watched to see if it moves out of the way before making any other decisions.
Complete Previa is the most dangerous and causes the mother to have to undergo a C section because the placenta is blocked the opening of the birth canal. It can be extremely dangerous and can result in hemorrhage if you try and deliver a baby vaginal with placenta previa.


Hey Hailey,
great job!
I saw that both your images show a more anterior placenta previa. I found some images that show placenta previa both anterior and posterior.

This first image ^ shows an anterior placenta previa that covers the internal os of the cervix

This image shows posterior placenta previa where the placenta covers the internal os of the cervix.
I didn't realize this was something to be noted until looking at images. Then I thought is one worse than the other? I found this study that shows if the placenta is more anterior it is more likely to migrate upward than a posterior placenta. The study shows a mean migration rate of 2.6mm/ week for an anterior placenta previa as opposed to a posterior previa that has a mean migration of 1.6mm/ week.
Here is a link to the study if anyone is interested!!
https://pubmed.ncbi.nlm.nih.gov/18067142/
Hey there Hailey !
Thank you for sharing those images, they are great, very clear examples of placenta previa. You response in which you said a placenta lying within 2cm is not as worrisome made curious. I’m wondering if the size of the baby can affect this at all? I’m curious if a big baby being pushed through that cervical canal can potentially cause hemorrhage even if it is two centimeters. What do you think ?
Hi Nailah! After researching I haven't found anything that mentions baby's size having anything to do with placenta position but I did see a few other things that can cause risk of placenta previa like scarring of the upper lining tissues of the uterus. Sometimes the placenta needs grow larger and compensate more because of multiple gestation, cigarette smoking in the mother, and living at high altitude which also causes a risk of placenta previa since its taking up for surface area.
Howdy everyone,
The location of the placenta is determined by where the blastocyst first touches the endometrium. The area of implantation where trophoblasts meet endometrium will become placenta. This area is called the decidua basalis on the mother's side and the chorion frondosum from the embryo's side. The placenta stays in one constant location and does not move throughout pregnancy; however, as the uterus enlarges the placenta appears to move.
The placenta is best implanted near the uterine fundus. If the placenta is near the internal os of the cervix (2cm or closer) complications may arise. Placenta previa may cause excessive bleeding and possible death.
This is a short video for us visuals.
https://www.youtube.com/watch?v=eMm6nCiK_no
Sarah
Hi Sarah!
Great post! I also watched the same video earlier this evening and loved how it was straight to the point with sharing key concepts. I love how you added the measurement of 2cm or less being a concern if that's the distance from the placenta to interal os of the cervix.
I also found this short video that helps further evaluate on placenta previa that I found to be of help.
Hi Sarah!
Thank you for sharing that video clip, I love videos that are straightforward and provide a clear understanding of the concept! One thing I found interesting about it was the causes of placenta previa. It mentioned a possible reason that implantation did not occur in the uterine fundus and thus resulting in a placenta previa could be due to fundal vascularity. It totally makes sense if the mother has had prior c-sections or uterine surgery, but it was the first time I heard anyone mention it! After all, we know the uterus needs to be highly vascularized to sustain a healthy pregnancy!
Hi Sarah!
I love your straightforward explanation! I agree that placenta on or near the cervix can be a big issue. However, did you happen across any studies on anterior placentas? What I've found were very contradicting on whether it would pose any extra risk to fetus. What do you think?
Karen
Hey Sarah,
Great response! I appreciated how you brought up the chorion frondosum. I recall coming across that in the lecture and my research as well. I’m still trying to connect the chorion frondosum and the chorionic villi together though. Are the chorionic villi essentially projections of the chorionic frondosum ? Curious to know your thoughts on this.
Hi Sarah,
You always have such clear explanations, I love it! As a fellow visual learner, the video you shared was super helpful, and I like how it explained the different potential causes of placenta previa. It got me wondering... is there any difference in the maternal experience with placental placement? Anterior placement makes it harder to feel fetal kicks, but does a particular placement provide less discomfort for mom?
I started researching, and found this article that states women with anterior placental placement are more likely to have lower back pain. I wonder why that is? Maybe because the baby's "anchor" is farther from the maternal midline and puts more counterweight on the lower back? I suspect it may all be equally uncomfortable by the time you reach the end of the 3rd trimester.
This article also noted that an anterior placenta may make a c-section riskier because the incision is more challenging.
The placenta will attach and grow wherever the fertilized egg implants. It's location will remain constant, however the placenta will grow with the uterus. There are many locations that the placenta can grow, like anterior, fundal, lateral, low lying, posterior.. and there are a few locations that would be a bad place for the placenta to be. Low lying, aka placenta previa, is not a good thing. This is when the placenta is low in the uterus and sitting on mother's cervix, and can cause bleeding during pregnancy and during childbirth, making it very dangerous for baby and mom. Anterior placenta can also be potentially bad, as there is higher risk of growth defects, placental abruption, intrauterine fetal demise, etc according to some studies.
These are two articles that go more into detail and are interesting reads:
https://www.verywellfamily.com/what-it-means-to-have-an-anterior-placenta-4690878
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3935544/
Hey there Karen !
I love those images! Too cute ! It’s interesting you brought up anterior placenta. I mentioned that in my response as well. I’m sure an anterior placenta may not be consider as great of a risk as placenta previa; but I wonder is this form of placental placement places a mother’s pregnancy in the high risk category as well? What do you think ?
Hi Hailey and Nailah!
I've looked and looked online to see what location for placenta is best, and there is no clear answer besides low lying being bad. Nailah, just like you I saw some articles saying there are risks for anterior lying placentas, but as I did more research, I saw that there are just as many articles trying to debunk it! Now I don't quite know what to think. This may be a great question for Dr. Wilson come class time!
Thanks ladies!
Karen
Hi Karen,
Great visual! I remember someone telling me that if the placenta is placed anteriorly, you are less likely to feel fetal kicks, which makes sense. A quick Google search [here] confirmed that fetal kicks are often felt much earlier in cases where the placenta is placed posteriorly. It also noted the added benefit of posterior placenta in that the fetus can grow in better alignment with the birth canal. Are there any different benefits to having an anterior placement?
Hi Karen! I love these pictures so much, they're so cute! I also learned that previa will be an indication of C-section for the mom and as you mentioned could be very dangerous for the mom and baby. Super important for us to document accurately when taking our images.
Hi Lania!
How exciting to be scanning OB patients. That's great your getting the eye for the placenta's location and knowing when its blocking the internal os. I hope that patient is in the clear when she returns for the f/u appointment! It definitely seems like she's at the stage in pregnancy where placenta previa is not something to take lightly so that's great it'll be monitored closely. I hope you're enjoying clinicals! It sounds like you're getting some great exposure!
-Molly
Hi Karen! I love how simple your images make the different positions! I thought from the lecture though that low lying placenta was a subcategory of placenta previas and not all low lying placentas create a marginal or complete previa... please correct me if I am wrong! If they are within the 2cm from the internal os, will they always have at least a partial coverage?
Thanks for any clarifications guys :)
Hey Lauren,
Great question! I feel like "low lying" is just a very general term that could potentially scare a lot of mom-to-be's. Here's a great article I found on "low lying placentas" and types of placenta previas.
Hope it helps answer your question!
https://radiopaedia.org/articles/low-lying-placenta-1?lang=us
-Karen
The placenta location is determined by where the blastocyst implants itself into the endometrium around 6 days after fertilization. Where the chorionic villi from the fetus and the maternal basal plate combine is where the placenta develops.
The placenta does not move from this starting location in the uterus during the pregnancy. It may change proximity from the cervix and surrounding landmarks due to the uterus both growing and changing shape, but it will always be attached to the same point. This is also why images of different bladder distention should be obtained in an exam; if the bladder is too full, it may make the placenta appear as covering the internal cervical os like a placenta previa.
A placenta that implants too low in the uterus has a higher chance of leading to complications, the most notable being placenta previa. Placenta previa may by low lying (within 2cm from the internal os), partial (covers part of the internal os), or total (completely covers internal cervical os). Term pregnancies with placenta previa should not be delivered vaginally as it puts the mother at high risk for bleeding, and a c-section should be performed.
I linked an article from the Mayo Clinic briefly explaining placenta previa. One interesting risk factor I did not think of was uterine scars, but that makes sense since there is less healthy tissue for the placenta to implant on in higher regions of the uterus. I know we are trying to stay away from pathology or complications for now, but it is a quick read to get us thinking!
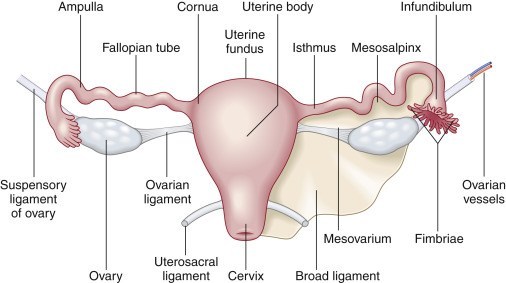
Howdy Lauren,
That's an excellent explanation of placenta implantation!
With all this talk of implantation/mechanisms I've been slipping on some basics! So, I like to remember (from last quarter) that the area of the uterus that connects with the fallopian tubes is called the cornua. Implantation closer to the cornua is better (since this means the placenta will be further from the internal os of the cervix.
Here's a quick reminder!
Sarah
Hey Lauren,
I enjoyed your response, great job! I like you how you took it a step further and mentioned how an overly distended bladder can essentially create a false positive for placenta previa. Do you understand how though? This image 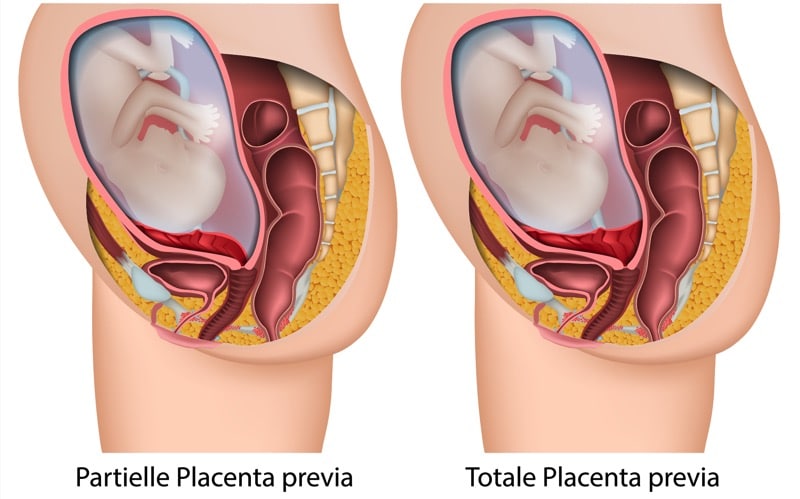
makes me think a filled bladder pushes upward, creating the illusion the placenta covers the cervix. What do you think?
A healthy placenta is an important part of a healthy pregnancy. The location of the placenta is determined by cells known as trophoblasts, which arise from the implantation in early placental development. The placenta can move throughout the pregnancy, but this is not so much as from the placenta actually moving but the uterus growing and shifting the placenta. Today in clinicals we did an OB survey scan on a patient that was about 23 weeks and she had a low lying placenta that was borderline placental previa. We scheduled her to come back for a follow up visit since the placenta can possibly shift on its own but if it doesn't, it would call for a C-section. I thought this was very interesting because it shows how important it is for us sonongraphers to pay attention to the cervix and placental tip to make sue they are not too close or the placenta is completely covering the cervix and birthing canal. So with that being said, we would not want the placenta to implant too close or block the cervical canal.

Hi Lania!
Thanks for sharing your clinical case! I haven't seen an OB patient with a placenta closer to the cervix yet. How soon did they schedule the patient for a follow up? I wonder how soon it is decided that the C-section will have to take place, how much time they will give the placenta to move further away from the cervix?
I found this image, showing a C-section through the placenta, I wonder if this is similar to how the patient in your case would have it performed?
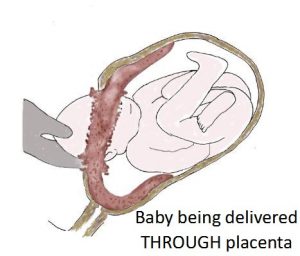
Hey Zuly,
It probably wouldn't go like this. When the cervix dilates in a placenta previa, the placenta will likely rupture. The mom would begin to hemorrhage before the she could push. However, is she wasn't in a hospital and had no knowledge of having a previa, I guess she would try to push the baby out no matter what. Unfortunately, I would assume the mom and/or baby wouldn't make it. Isn't it crazy to think that something like a previa has a pretty simple solution today, but could have been a death sentence 100 years ago?
Hey lania,
You worded your response really well! Great job! I am glad you are getting experience with OB at your site. Are you noticing at your site that beyond the 20 mark and as the baby gets bigger, their anatomy becomes more difficult to recognize?
Hi Naiilah! Thanks love! And yes, I've totally noticed that. I asked my CI why that was so, since in my mind I thought the baby would be easier to see as they got bigger, but she clarified that actually around 20 weeks is most optimal because they are still small enough to move around freely and have space, compared to a baby further along in gestational age that is in a since outgrowing the uterus. Having more space for amniotic fluid when the fetus is around 20 weeks helps have a better window to identify baby's anatomy. I thought the complete same thing as you! LOL
Hi Lania,
Thanks for sharing your clinical experiences! I am wondering if you were familiar with this patient's history? Do you know if this was her first pregnancy, or if not has she had a history of placenta previa with other pregnancies? Hopefully she gets good news at her follow-up exam!
Hi girly! I actually did check for patient's history, and this was her first pregnancy, so I couldn't relate it to another pregnancy, but I had the same thought process as you! If I happen to have another patient with the same or similar condition I will check again and let you know if I found any correlation. :)
Hi Lania!
Thanks so much for sharing your clinical story! I asked my CI the same thing, along the lines of "What can a PT do if they have placenta previa?" and he gave me the unfortunate news that there's nothing you can do to move the placenta around. I can't image if you guys missed that and the mother went into labor. I've heard stories of mothers being in labor for > 12 hours and just ended up in a c-section.
Our career is so rewarding! We must be vigilant for doctors to safely deliver these babies!
Hey guys! Here's something to consider:
Sometimes during an exam, the baby's head is so low that it is difficult to evaluate the internal os. You wait and wait for the baby to move, but the little angel is just cozy where they are. You notice the placenta is in the lower uterine segment and can't definitively rule out a previa because the head is obstructing your view. What do you do?
Hi Paris,
That's a great question! I am wondering if a translabial imaging technique might be helpful in this instance? I remember Dr. Wilson mentioning in this weeks lecture on the Cervix that it provides us an in depth look at the cervix without the invasiveness of a transvaginal exam! I'm sure there are more ways to evaluate, but this was the first thing to come to mind!
Hi Paris!
Great question. Perhaps you could ask the mother to walk around (if it's safe for her to do) and see if this would cause the baby to move positions?
I remember when I was shadowing there was a case like this where the baby wasn't in a good position to get a good images and the tech made the mom walk around the building and even do squats!
I don't think the mom was thrilled about having to do exercises... but the baby did end up moving positions :)
Hi Paris! I saw this and had to comment lol, I want to say translabial because at my site, the tech I was following told me to start an OB my first week even though I had no idea what I was doing. I knew I had to find the cervix because I had watched it before that so i went looking. Shocker... I couldn't find it. The tech came and she also couldn't see it! She ended up doing translabial and got a beautiful image.
Hi Paris!
I found this article that explains some possible options to visualizing the cervix since it may become more difficult to visualize it as the third trimester approaches. It mentions options like external fetal manipulation, overdistension the maternal bladder, and Trendelenburg position, as ways to better visualize the cervix, however it also says these options may distort the cervix. and also obviously be uncomfortable and not ideal for the patient. The article explains results of a study done of the effectiveness of transperineal ultrasound in cervix imaging, here is a quote with some results:
"The entire length of the cervix was seen in 136 (86%) of the 158 patients scanned transpenineally. In the remaining 22 patients, the internal os and upper portion of the cervix were successfully visualized, but the external os and caudal portion of the cervix were not seen because of shadowing from gas in the adjacent rectum."
So it definitely seems like a great option when it is difficult to visualize transabdominally!
https://www.ajronline.org/doi/pdf/10.2214/ajr.157.1.2048542
Hi Paris!
At my clinical site, we are constantly asking the momma to be to move LPO to RPO if the baby isn't in a good position to find the best represented image during the scan. If the baby still stays within that same position, we may also have the mother use the bathroom or walk up and down the hall for 5 mins. Once the mother returns from the bathroom/ walk, the baby's position typically changes and it accurate for imaging.
Thanks for that challenging question! You can never NOT learn something new with this modality! So many tips and tricks to learn, I love it!
