Typically it's the third trimester when some of these complications (whether maternal or fetal) will really start to express themselves. As sonographers better understanding the fine line of keeping a fetus in the womb for as long as we can, vs getting them out as the environment is no longer suitable to thrive- what are ways we can help to monitor the situation with sonography? When do we do studies, what are we looking for, what diagnostic and therapeutic tests can we aide with, which invasive procedures may help with certain situations...
Discussion Board Week 9.............
What we can do as sonographers is thoroughly assess the maternal and fetal environment with the study. Specifically, we usually scan moms in their third trimester when something is going wrong, such as IUGR, placenta previa or placental abruption. At my site, we have a rule to scan biometrics if the last scan was over 10 days. I think this is a great way to regulate every sonographer into monitoring these 3rd trimester scans. If the order is to monitor placenta previa, not only do I want to fully assess the placenta and its tip to os, but I want to take a look at the biometrics of the baby. This gives the radiologist more information of not only the location of the placenta but how well the baby is thriving. Doing the bare minimum of only looking at what the order was for is naive in my opinion.
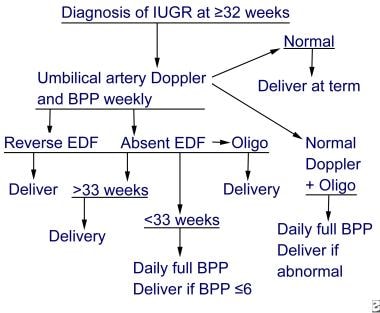
When we are doing studies, we are looking at biometrics, Doppler ratios (if something is askew or IUGR is noted), and the maternal environment. Biometrics get a little more tricky and less accurate (BPD in particular) in the third trimester due to growth/molding of baby and less amniotic fluid. One of the therapeutic tests sonography can help with is the Biophysical Profile. While this is mostly done by nurses, sonography is used to aid in the scoring process of this test. With sonography we can see fetal body movement, fetal tone, fetal heart rate, and amniotic fluid. The 5th parameter is fetal breathing, this is a little more challenging but can still be evaluated with sonography in the third trimester by observing the movement of the diaphragm. A normal score is 8 to 10, however if an abnormal score of 0 to 2 is observed the patient will be scheduled for immediate delivery. This is just one of the ways that sonography aids in the quality of life for these babies (specifically in the 3rd trimester).
I found this chart to be interesting. It sums up what I have mentioned here and the outcome of baby's delivery date depending on our findings in sonography.
Great chart Amanda---two things come to mind 1) I'm surprised your site will rescan all biometrics after 10 days. I always followed the rule that you never rescan measurements unless there have been at least two weeks between scans for these reasons: every sonographer will measure slightly different, and in the third trimester there are so many averages going on, that those slight differences can actually make the baby look as if it has shrunk if done too soon, and 2) fetuses like neonates and children go through these massive growth spurts...and you don't know where they are in their cycle--so if you measure too soon, they might be on the verge of a big growth spurt and miss it. Needless to say, you should follow what your lab's protocols are-I have just never done it before 2 weeks interval.
The second idea on your post (which thank you for posting), is your comments on BPP's.....you are correct in that this is mainly done outside of radiology. We used to perform them all the time specifically for the reason of fetal well being- but now RN's typically do them up on the floor. In fact, I haven't seen a request for a BPP for years...however, as sonographers it is incredibly important to tie as many pieces of a patient's puzzle together when we get the change. So...every single time I perform a third-trimester growth scan and the growth is off even slightly (like growth 20th centile instead of below the 10th centile), I will always perform a Doppler study beginning with the Umb Arts, then the MCA, then do an official AFV (all 4 quads not just the DVP), then I ALWAYS throw in a BPP. Again it's about painting the picture that explains the diagnosis I'm trying to make. As a sonographer you always have to pick a side...the GB has stones- I don't say it outright, but I corner the interpreting MD into having to say it....echogenic mobile foci that shadow, dilated CBD, pericholecystic fluid, +Murphys sign....I'm not stating it...I'm just sayin with my pics.......
A baby that is not thriving has serious implications- like cholecystitis- someone has to do something and do it now....I'm not saying it outright but I'm showing you that the fetus is <10th centile, the AFV is 4.3, the BPP is 4/8, the UA S/D ratio is 5.4 and the MCA is 2.3....I'm not about to diagnose but I'm giving you all the goods to tell the OB to get this baby out. I have had to scan third trimester OB studies from L&D on countless occasions where the perinatologist or OB that is about to deliver is breathing over my shoulder for me to answer those questions...they are immediate as they can be life-saving for multiple people (baby and mom, and really the entire family that just expects a fantastic outcome instead of losing two members of their family) and even before the radiologist gets to review the images and dictate a report- the baby is already delivered based on what my scan that they watched showed. So please, please really try and understand all these parameters that contribute to a good or bad outcome.
Does that make sense- good job posting Amanda.
Hi Michelle,
I shadow a handful of techs and lately I've been with one who has been scanning for years (and tends to do their own thing) and he does biometrics after 10 days. All the other techs perform biometrics after 2 weeks, so I think this is the correct protocol for our site.
We have had a handful of third trimester limited OB scans, most for IUGR & fetal pyelectasis. With the IUGR scans, some orders will request Dopplers. If we do umbilical artery Doppler and it appears to have a normal S/D ratio, would you still Doppler MCA to show the Radiologist you checked all the parameters? I would think maybe not because we want to reduce exposure to the baby. On the other hand I wouldn't want to miss an abnormal MCA S/D ratio.
Thank you for responding!
I have had a few third trimester scans this month. Mostly they are for size/date discrepancy. Typically due to fundal height measurements from the OB, but also maternal history/previous pregnancy complications contribute to further monitoring. Third trimester scans are optional and usually ordered when the pregnancy is already considered high risk. Like Amanda and Michelle mentioned we do biometrics if the previous scan was done more than two weeks prior. We always look at the cervix, placenta, heart rate, and fluid levels. If the fetus falls below 10%, % has dropped significantly, or dopplers were performed prior we will also doppler the cord at the abdominal insertion, cord in fluid, and at the placental insertion.
By the third trimester IUGR will be more obvious than at the 20 week screening, specifically asymmetrical IUGR. The fetal head may measure accurately but the abdomen will be measuring low. This finding would call for cord dopplers to show the reading radiologist what we are seeing. If reversed flow is documented the reading radiologist should be contacted before the patient leaves. We had this happen once and were directed to send the patient to labor and delivery for further monitoring. As we learned before once cord flow begins reversing the fetus has on average 7 days to live, the problem is we don't know if we are seeing the drop out on day 1 or day 7.
If polyhydramnios is the issue therapeutic amniocentesis can be performed. The AFI will be documented and the sonographer will aid with needle placement for the safest area to draw fluid from.
Another interesting note that Sue added on my site visit is that she liked to add the 4 chamber heart view to all of her OB studies. This is not something that is currently in my protocol, but she brought up the point that some pathologies are more obvious later in pregnancy that may have been missed on earlier scans. The work we do during these studies saves lives. If pathology is found it gives the mother time to consider options and set up a delivery plan with the appropriate staff. If pathology is missed (placenta previa, heart defects, IUGR) the outcome can be life or death.