Let's use this thread to dig into the lung pathologies we most commonly will run across in our sonographic evaluations.... Can you provide examples and discussion around topics of interest.
Discussion Board Week 6.............
I chose to elaborate on bronchopulmonary sequestration (BPS)
The following images are from The Fetus (link posted below) this BPS was noticed at 24 weeks, the mother had no contributing history. The color images below show the feeder vessel, which is how to differentiate this pathology from a grade III CPAM. Sonographically BPS will be hyperechoic and may be difficult to differentiate between normal lung tissue. Although they mimic lunch tissue they have no connection to the airway vasculature and as demonstrated below will have a separate feeder vessel.
These masses can be intra or extralobar. It is imperrative that these lesions are caught in utero so that the correct surgical team can be prepared after birth to extract it. If the mass (benign) is large it can severely interfere with breathing.
Here are some additional stats from https://radiopaedia.org/articles/pulmonary-sequestration
- intralobar sequestration (ILS)
- accounts for the majority (75-85% of all sequestrations 4,5,7)
- present later in childhood with recurrent infections
- extralobar sequestration (ELS)
- less common (15-25% of all sequestrations 4,5,7)
- usually present in the neonatal period with respiratory distress, cyanosis, or infection
- recognized male predilection M: F ratio ~4:1
- can be infradiaphragmatic in ~10% of cases




Hi Heatha,
Thanks for the pictures, that is for sure a feeder vessel in the lesion, giving the radiologist way more detail to the story of this little one. This may sound stupid but I was trying to look up the definitions of interlobar and extralobar. I know that interlobar is between two organs, but is extralobar similar to exophitic? Where the lesion is hanging off one organ?
I wanted to touch on Congenital Cystic Adenomatoid Malformation (CCAM)- also known as Congenital Pulmonary Airway Malformation (CPAM)- since I wasn’t familiar with the different types. I know when we are in the field we just describe what we see in our impression and won’t be saying the specific type of CCAM we are documenting.
Type I congenital cystic adenomatoid malformation
· single/multiple large cysts, 2- 7 cm in diameter
· smaller cysts can also be found
· alveolus-like structures, much larger than normal alveoli can be seen adjacent to or communicating with the larger cysts
Type II congenital cystic adenomatoid malformation
· smaller cysts, usually less than 1 cm
Type III congenital cystic adenomatoid malformation
-
· firm, bulky masses of lung tissue
· usually consisting of small cysts
So, basically, the characteristics of the cysts start big (type 1) and get smaller (type 3). Since the cysts in type 3 are so small they appear as a bulky mass of lung tissue. According to TheFetus.net, there are different stages in embryology of when the lower respiratory system forms. I found this to be interesting, especially with the formation of type 2 because we could do a 20 week survey and the Type 2 CCAM can still form after, up to week 26.
My source says that Type 3 CCAM forms at the pseudoglandular stage where bronchiolar division occurs [5-17 weeks gestation].
Type 2 CCAM forms at the canalicular stage where the beginning terminal sacs develop [16-25 weeks gestation].
The images shown below are of type 1 CCAM. You can see how large these cysts are, especially in the MRI image.
That CPAM is huge! Did the case study say whether the baby survived? I'm wondering if because its so large if it compromised lung or heart development in utero to the point where it can't be fixed after birth. So if I understand you correctly type 1 are the largest and develop early, type 2 are sneaky and can develop after the 20 week anatomy scan and type 3 are microcysts that prefer the bronchioles and develop before 17 weeks?
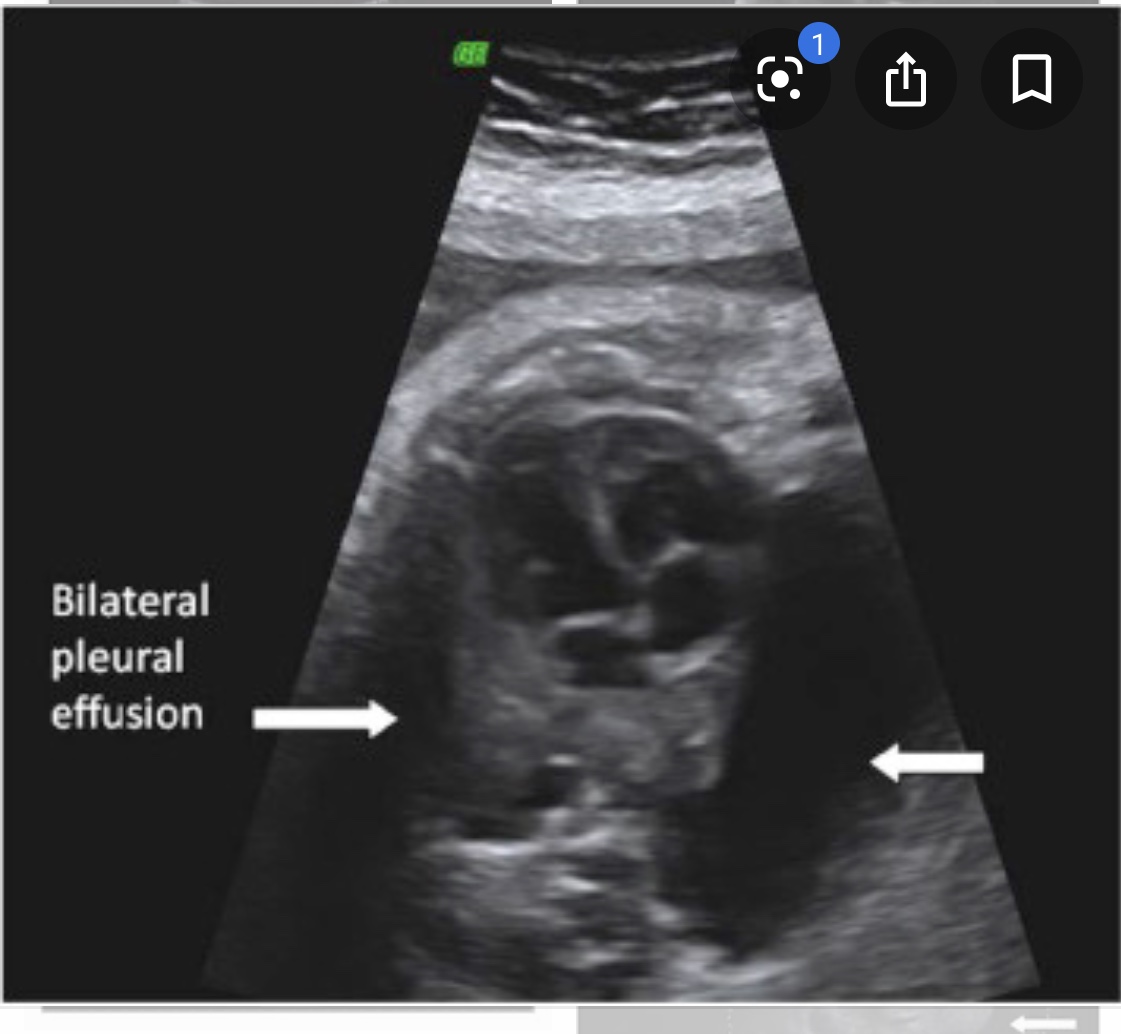
I wanted to learn more about fetal hydrothorax or pleural effusion so I did some additional research. This is only referring to fluid that accumulates within the thorax. The fluid can compress the lungs and shift the heart into a abnormal position. Do not get this confused with pericardial effusion which is fluid in the heart. I had a hard time separating the two, so I thought I’d write it out and talk about it once more to be sure it sticks. =)
https://www.sciencedirect.com/science/article/abs/pii/S0009926098801888