There are multiple conditions and stages that occur with a first-trimester pregnancy. How can we tell the differences between presentations and normalcy? Include an image to explain your answer.
There are multiple conditions and stages that occur with a first-trimester pregnancy. How can we tell the differences between presentations and normalcy? Include an image to explain your answer.
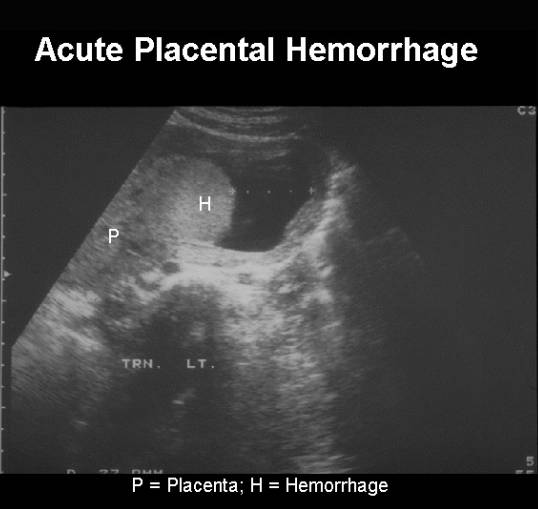
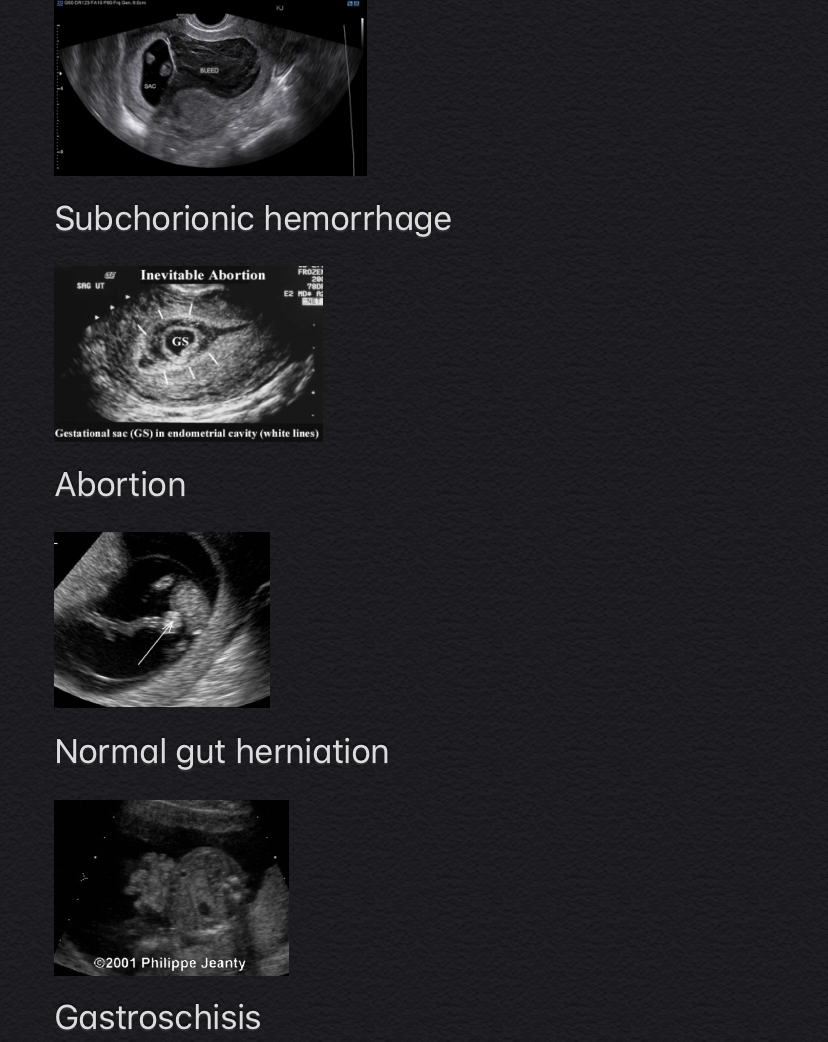
There is a common occurrence of subchorionic hemorrhage that causes bleeding / spotting. There is placenta hematoma that is hard to distinguish sonographically between the two. However to differentiate the subchorionic hemorrhage bleed is outside the chorion sac. Hence patient is bleeding. Placenta hematoma is contained within the chorion so patient should not experience bleeding. In addition another that comes to mind is fibroids and uterine contractions. Simply revisit the area of interest within 20 min time frame and if the "fibroid" disappears it is simply a uterine contraction.

Hi Charissa!
Thanks for sharing about subchorionic hemorrhage and placental hemorrhage. It important to note the location of the bleed in relation to the placenta to rule out placental hemorrhage.
Another differential for the 2nd image is twin gestation. Although that can be misdiagnosed due to a hematoma being large enough to mimic the size of the gestational sac. In that case we can differentiate the two diagnoses by being aware of the consistency between the two fluid collections. If one fluid collection has a fetal pole and yolk sac and the other does not it may be indicative of a normal presentation of a hematoma. Or the twin gestation diagnoses could be fact and the presentation is abnormal where one embryo did not form leading to possible diagnoses of twin transfer, abortion, or blighted ovum. And hCG levels definitely play a part in diagnosis.
Hi Jackie good call on the twin gestation! I didn't think of that correlation. Also we could look at the AFP levels to determine if its a potential differential for twin gestation. If they are not elevated we can rule that out. Identifying the size of the hematoma is helpful because it can provide us clues of what potentially can happen as you mentioned above, spontaneous abortion, blighted ovum, but also if they are small a better outcome.
I appreciate your feedback!
Hi Charissa,
Thanks for pointing out that with placenta hematoma there will be no bleeding, but with subchorionic hematoma there will be. Just a simple reminder 25% of pregnancies result in bleeding during the first trimester and about 50% of those will miscarry. This can be quite scary for mothers to experience.
According to an article from, VeryWell Family, " Under most circumstances, women who develop subchorionic hematomas enjoy otherwise normal pregnancies and go on to have perfectly healthy, happy babies." This makes me happy!
Do you know what the risk of of complications are, related to a subchorionic hematoma?
Hi Maria!
Yeah I was able to scan a OB patient who came in for bleeding and it ended up being a subchorionic hemorrhage. My CI said it was a common occurrence and didn't seem alarmed. This was before we even learned about this type of hemorrhage, so I was confused of why she was so nonchalant about it. It makes sense now because of the accumulation of the blood between the uterus lining and the chorion. As for complications of subchorionic hemorrhage, according to "Medscape," they mentioned an increase risk for placental abruption, miscarriage, or spontaneous abortion.
https://www.medscape.com/answers/404971-42151/what-are-the-pregnancy-risks-associated-with-subchorionic-hemorrhage-subchorionic-hematoma
Hey charissa-
I'm so glad we are starting with subchorionic bleed. The one and only first trimester I saw at my site, I now realize this patient probably had one. At the time I was so excited because I thought the patient was having twins! I remained calm and kept my poker face. When my CI and I left the room I immediately looked at her and said, "Twins?!" She let me know very quickly that it was not a viable pregnancy (singular). At that time I didn't realize what the second 'gestational sac' was. Now thinking about it, I bet it was a subchorionic bleed. It was two cystic sacs that were just adjacent to each other and neither with a yolk sac (which by that time) there should have been one.
This is crucial to be able to identify a subchorinic bleed from a pseudosac from a gestational sac and so on.
Thanks for the share!
It is important to use dates, labs, and clinical history to differentiate between abnormal and normal presentations.
For example:
At 4 weeks this image can have many differentials: pseudo sac, blighted ovum, possible gestational sac, cyst. The time is too early to tell whether or not it will be a normal pregnancy if a patient is hCG positive. So our job would be to describe while the radiologist may dictate based off of hCG levels. At this early time things appear normal because there is not enough information. What we don't know is if there is an ectopic causing a rise of hCG levels or if this is a normal IUP.
If this image is taken at 9 weeks then differentials are more towards pseduo sac or blighted ovum, because there is no fetal pole or secondary yolk sac. Dating makes a difference. If hCG levels are non existent then this can be a normal pseudo gestational sac. If hCG levels are high then it can be an abnormal blighted ovum.
Hi Jackie,
I strongly agree that "dates, labs and clinical history," is an important factor for differentials. I was so blown away today when learning that all we can really do is describe the fluid collection without being able to know what it truly is. Abnormalities can be very tricky. It was a little hard for me to keep up and correct me if I am wrong, pseudo sacs result from a blighted ovum? And will the blighted ovum or pseudo sac resolve on its own?
From my understanding, a pseudo sac is any fluid collection within the endometrium/myometrium that mimics the appearance of a gestational sac. A blighted ovum is a genuine gestational sac that has not formed an embryo so it will inevitably abort. This blighted ovum can fall under that classification of a pseudo sac, because a viable pregnancy is not identified due to the lack of secondary yolk sac and pole. But a pseudo sac is not necessarily a blighted ovum. For example an ectopic pregnancy can cause the uterus to secrete fluid in the form of a pseudo sac but the implantation could not have occurred. So the pseudo sac in the uterus is not a blighted ovum. It's just free fluid. Please correct me if I'm wrong, anyone. But that is my understanding.
In addition, I found this site that explains the pseudo gestational sacs more thoroughly. According to radiopaedia.org :
A pseudogestational sac, also known as a pseudosac or intra-cavitary fluid, is the concept that a small amount of intrauterine fluid in the setting of a positive pregnancy test and abdominal pain could be erroneously interpreted as a true gestational sac in ectopic pregnancy.
https://radiopaedia.org/articles/pseudogestational-sac-1?lang=us
A thick decidual layer can still surround a pseduo gestational sac, but the sac could give itself away by having an irregular border. They call that "beaking."
Hi Jackie,
I completely agree that dates, labs, and clinical history are absolutely vital to the list of differentials and which way you’re going with the picture you’re trying to paint for the radiologist . My concern is what happens when the woman comes in with irregular people or the one with the unreliable memory. Then the picture becomes murky because are the lab values off due to a problem with the pregnancy or because the information given was off? Is there a time when we don’t necessarily listen to the patient and go with the pictures and lab values? This is my biggest concern with blighted ovum versus pseudo sac and others.
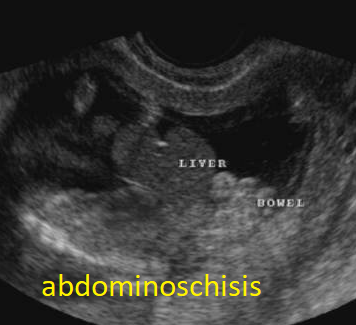
Normal midgut herniation versus abdominal wall defects
Normal midgut herniation in the base of the umbilical cord usually starts at 8 weeks of gestation because midgut loops grow faster than the abdomen and they need to rotate as well. Starting that time we can easily visualize midgut herniation by ultrasound.
Sonographic appearance of normal midgut herniation:
If we see midgut herniation in the base of umbilical cord after 12 weeks of gestation, we might suspect limb-body-wall complex, gastroschisis or omphalocele.
In the image on the left we see normal gut herniation (embryo is 9 weeks gestation), On the image on the right we see that the gut herniation is persistent and it is not normal finding. It is omphalocele.


Hi Ellen,
You did a wonderful job explaining the normal mid gut herniation versus the abdominal wall defects. Can you help me identify the differences between the 3. I know with Omphalocele the herniation protrudes through the navel and with Gastroschisis it protrudes besides the belly. How is the limb-body wall complex described?
Hi Maria,
Limb-body wall complex is a rare lethal condition, characterized by severe fetal malformation and a very short umbilical cord. It can be caused by maternal drug abuse (cocaine), early vascular disruption, and severe amniotic band syndrome.
Fetal anomalies will be obvious on sonographic evaluation:
For more detailed information, please look at http://www.fetalultrasound.com/online/text/8-013.HTM



Ellen,
You did a magnificent job outlining the normal process of the midgut herniation and abdominal wall defects. It is understandable why the CRL is used in dating after it is obtained instead of relying on inaccurate dates, especially when it comes to normalcy versus pathology and how ones care may continue down the road. I can appreciate how much of our job is obtaining normal picture, while staying alert and using critical thinking for the times when it’s not.
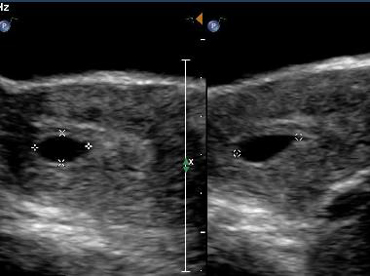
Hi Class,
Today we covered a great amount of information on 1st trimester abnormalities. I will be modifying this thread throughout the week. I'd like to add that LMP is one of the most important dates to obtain from the mother. The LMP will help us identify if something is in fact abnormal or normal and what to look for when scanning. Fetal rhombencephalon, which is an anechoic structure at the posterior part of the brain normally happens within 8-10 weeks and is a normal appearance, but can mimic Dandy-Walker malformation, which is an enlargement of the posterior fossa, a rare congenital malformation of the cerebellum and fourth ventricle, so it is super important to know the gestational age when imaging. I often think about being in a room with a patient and getting nervous if I seen such an abnormality. I have to remind myself to "go with what you know, " which is the basic steps. I know in time we will get use to it and we will know exactly what to describe but being that it is so new, I want to make sure I understand what I am up against.
I'm looking forward to see what we can come up with this week! Remember, all questions are good questions, and as the moderator I encourage us to lean on each other so we can better understand the material.
The first picture is a normal appearance of the fetal rhombencephalon. The second image is picture of Dandy-Walker malformation.


Hello Maria,
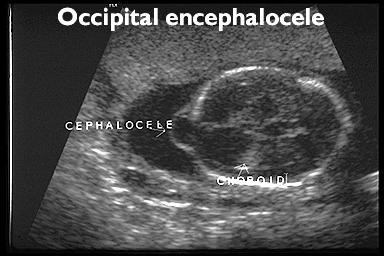
After reading your post guess what came to mind? the cephalocele and cystic hygroma. i brainstorming of all the CNS abnormalities however these two kinda stuck with me.
The cephalocele is an abnormally in the fetal brain resulting from the calvarium not closing properly and as a result the meninges are not correctly encapsulated. It will appear as a solid mass with a protrusion of the skull. It is so important to take our time with the skull and not miss any pathology.

The cystic hygromas on the other hand are a sac filled with fluid so it will appear anechoic. Cystic hygromas usually derive from the fetus having a lymphatic system problem. The cystic hygroma will appear around the neck on the posterior side and also around the upper thorax. During exams having our gain and TGC at an appropriate level (optimizing) can help us get better images and help us determine sacs from calcifications.

Great differential Jazmin. Cephalocele might even be a differential to rhombencephalon, given that they both protrude near the brain. I agree with both points you've made. Taking our time is key, we don't want to rush the process and miss something. Also, TGC is our best friend, we need to make sure we are telling our story to the radiologist with our optimized images.
I wasn't really sure what meninges meant. I looked it up and found that they are a complex connective tissue surrounding the central nervous system (brain and spinal cord).
Here is an image that show the 3 layers of the meninges: Dura mater, Arachnoid and Pia Mater.
Hi Jasmin,
I like your example and explanation. For general purposes, I just would like to add that cephalocele may involve also frontal, parietal, orbital, nasal, and nasopharyngeal regions of the head in addition to the occipital region. We need to remember, that in the Western hemisphere most commonly will be seen cephalocele due to the occipital cranial defect, and in the Eastern hemisphere, in the opposite side of the globe, cephalocele due to the frontal cranial defect (in the opposite side of the head). I uploaded several sonographic images and pictures of babies with cephaloceles of different locations. It might help to understand and remember them better.


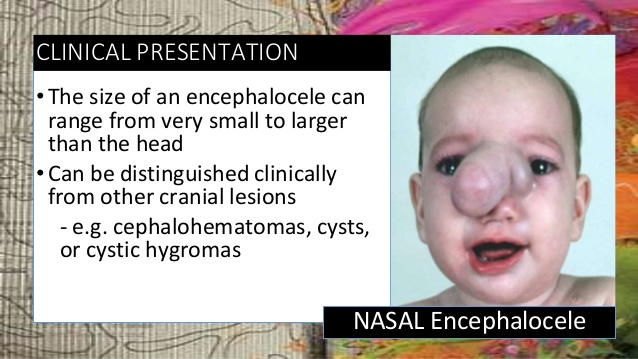

More information on nasal cephalocele you can find here https://childnervoussystem.blogspot.com/2017/07/nasal-encephalocele.html
Hey Maria-
Thanks for comparing those two! Some CSP is okay, but too much is worrisome. Just remember that we are not really supposed to diagnose Dany Walker Malformation until the 2nd trimester. This is because there could be a false-positive diagnosis can be made at gestational ages of less than 18 weeks.
"Cerebellar malformations, particularly subtle findings such as Dandy-Walker variant, should not be made at less than 18 weeks gestation because it is possible that the development of the cerebellar vermis is incomplete."
However, it would be super important for us to document our findings a bit more than we normally would. This would let the radiologist know that we are seeing something a bit abnormal at this time.
Here's the site in case you'd like to read a bit more about it. https://rarediseases.info.nih.gov/diseases/6242/dandy-walker-complex/cases/52163
There are so many things to look for to confirm a first trimester pregnancy. Obviously we should first be looking at the qualitative and quantitative hcg levels. In early pregancy the uterus may appear enlarged with a gestationsal or pseudosac in the endometrium. Another positive indicator of pregnancy is the presence of a corpus luteal cyst, it is not required, but it does support the presence of a pregnancy. However there is also the possibility of an ectopic pregnancy, which closely resembles a corpus luteam cyst.
I found this case detal below from sonoworld and read another comparing the resistive index's of an ectopic vs corpus luteum cyst. https://sonoworld.com/CaseDetails/Ectopic_pregnancy.aspx?CaseId=60
below is the corput luteam cyst with the "ring of fire"

Followed by an early ectopic pregnancy and the "ring of fire"

Both of these images are from the same case study.
They both show a ring of increased vascularity. It is difficult to distinguish an early gestational sac from a normal corpus luteum cyst. Some suggest the gestational sac will be more echogenic than the compared ovarian tissue. Another comparison will be to look at the resistive index of blood flow. There is a summary below that I am still making sense of. The overall takeaway is that the ectopic pregnancies showed a resistive index of greater than 0.7. https://www.ncbi.nlm.nih.gov/pubmed/14620888
If the findings were inconclusive a patient would have serial scans and blood draws to monitor the pregnancy. Eventually if a yolk sac was seen then an ectopic pregnancy could be confirmed. If no ectopic was found either it was an early demise with corpus luteum cyst or the pregnancy was too early to see in the endometrium and a true gestational sac with secondary yolk sac would be observed.
Hello Heather,
This is a great example of how the corpus luteal cyst can be confused for an ectopic pregnancy. I also had a hard time distinguishing the difference in quarter three. Another, way you can tell the difference in addition to checking the pregnancy test and HCG levels is by asking patient history, because if she has a history of ectopic, cesarian, or heterotopic pregnancy than evaluate further for another ectopic.
While reading your response I thought about the Theca Lutein cyst which are common in first trimester molar pregnancy. Theca lutein cyst are usually bilateral, they are caused by increased level of HCG due to the molar pregnancy. It is so important during all of our OB anatomy scans to always look at the mothers anatomy because evaluating the ovaries during a first trimester could give you lots of information. I read that the Theca lutein cyst are commonly incidental finding which, kinda goes with Dr. Michelle's story.
Massive Theca Lutein cyst

Whoa heather.. the ring of fire around corpus luteum cyst and ectopic pregnancy is a hard one to differentiate. I tried reading the summary on resistive index and like you, I'm trying to make sense of it. A patient came in the other day and had a cyst in her ovary, she didn't have her period for 3 months, but her hCG levels didn't indicate a pregnancy. I was trying so hard to figure out what was happening. She was in pain and bleeding. My first thought was an ectopic pregnancy, but because her hCG levels weren't matching, I thought an abortion. She did have free fluid, so thenI thought a ruptured cyst. I was so curious and even the tech couldn't call it. I'm actually going to go back and review the report, because I want to know what the radiologist called it. These differentials sure are tricky.
Hello Heather,
i'm glad you choose this topic specifically the corpus luteum. This week in clinicals we had a referral for ED patient early pregnancy .I got excited as I don't see much ob let alone first trimester. Reason of referral was to rule out ectopic due to bleeding. We went over priors. Sonographer and I were making hypothesis as to what it could be. Upon scanning we did see what we thought was the corpus luteum pop some color on there and the ring of fire surely enough confirmed it for us. Its great to know foundation as the corpus luteum could have easily been mistaken for an ectopic especially in early pregnancy as both due have increased vascularity thus looking the same via sono. I will most definitely remember to distinguish one from another is to compare RI as ectopic has greater RI of .7. Thanks!
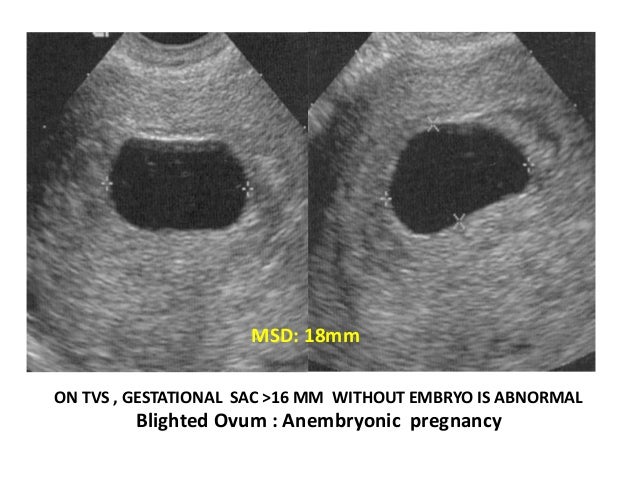
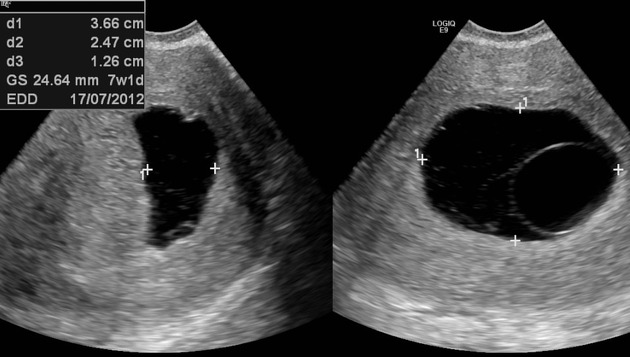
A failed pregnancy due to a blighted ovum can be visualized in the first trimester. This happens when a normal looking gestational sac doesn’t have an embryo because it either didn’t start developing or stopped developing very early before it could be documented with ultrasound. In these situations the gestational sac may continue to grow without the embryo for some time and the hCG levels might continue rising. The best way to prove this is with knowing normal values and give it time. We should remember that in a normal pregnancy the mean sac diameter increases by 1.13mm a day and anything less than that is not ok. The bottom line is that a Mean Sac Diameter of 16-24 with NO embryo is a suspicious finding and a MSD of 25mm+ with No embryo is suggestive of a failed pregnancy.
It is recommended to asses the pregnancy in 7-10 days after finding the contents of gestational sac suspicious.
information resource: Hagen-ansert textbook, chapter 50.
VS a normal Gestational Sac for its dates

Hi Elona,
These first trimester complications are terrifying. I never realized how many failures are possible during the first trimester. Thank you for reminding us of the measurements of the MSD, this is important to understand so we can accurately asses the scan. It just blows my mind that with a blighted ovum, the placenta will continue to grow and support itself with no embryo.
I found this blog online about a woman who has experienced a blighted ovum and several miscarriages there after, very saddening that once you have an abortion or miscarriage, the body is at higher risk of getting another. She failed 6 times, but is not giving up. Check it out!
https://www.miscarriageassociation.org.uk/story/ninas-story/
 The way to know if a first trimester pregnancy is normal or pathological we need to have a good foundation on what normal looks like. We know that the ideal pregnancy will be in the uterus with a decidual reaction caused by the surge of hormones. If it is a pregnancy it will have a combination of lab values, such as, HCG levels and on ultrasound we will see a gestational sac with the secondary yolk sac and an embryo. If this were to be pathological we would have to make a hypothesis of what could be wrong with this pregnancy. We can possibly see an abortion, a molar pregnancy, some anomalies that are present in the first trimester, and molar pregnancies. When the blastocyst implants in the uterus and the trophoblasts is digging its way through a mother can have bleeding which can be normal or abnormal. Normal would be a little bit of subchorionic fluid, and abnormal would be seeing fluid around the whole gestational sac which could be indicative of an abortion. Also, we should not confuse a normal with pathology. If we are scanning a 10 week old embryo and see that the stomach looks like it is protruding we don’t want to call it gastrischisis or an omphalocele because between 9-11 weeks it is normal to see this on an embryo because of the intestines rotating.
The way to know if a first trimester pregnancy is normal or pathological we need to have a good foundation on what normal looks like. We know that the ideal pregnancy will be in the uterus with a decidual reaction caused by the surge of hormones. If it is a pregnancy it will have a combination of lab values, such as, HCG levels and on ultrasound we will see a gestational sac with the secondary yolk sac and an embryo. If this were to be pathological we would have to make a hypothesis of what could be wrong with this pregnancy. We can possibly see an abortion, a molar pregnancy, some anomalies that are present in the first trimester, and molar pregnancies. When the blastocyst implants in the uterus and the trophoblasts is digging its way through a mother can have bleeding which can be normal or abnormal. Normal would be a little bit of subchorionic fluid, and abnormal would be seeing fluid around the whole gestational sac which could be indicative of an abortion. Also, we should not confuse a normal with pathology. If we are scanning a 10 week old embryo and see that the stomach looks like it is protruding we don’t want to call it gastrischisis or an omphalocele because between 9-11 weeks it is normal to see this on an embryo because of the intestines rotating.
Hey Lauren,
Much agreed that we should know what normal is and if we see something that is questionable we should speak up. Capturing the images and having help from our cohorts is better than missing something that can be pathological. According to Medscape. "Sonographic visualization of a subchorionic hematoma is important in a symptomatic woman because pregnant women with a demonstrable hematoma have a prognosis worse than women without a hematoma. However, small, asymptomatic subchorionic hematomas do not worsen the patient's prognosis." So although, it is quite scary to have subchorionic hemorrhage, it is safer to have a smaller one that will hopefully resolve on its own.
As far as the normal gut herniation, do you remember what week it should resolve by?
The most important information to obtain during a first trimester OB ultrasound is patient’s LMP, hCG levels, any screening tests, and even patient’s age. While reading the chapter, I noticed a lot of these pathologies are associated with an advanced maternal age. I don’t know about any of you ladies, but I when I look at the order for an OB study I instantly look at age because I know if the mother is over 35 I should be expecting some kind of anomaly during the exam (and I do not mean this in a negative way, of course I hope to scan a healthy baby).
A way we can tell the difference between pathology and normalcy is coming back to scan an image after already taking it for the first time. For example, during a first trimester ultrasound we may see an enlarged mass on the uterine wall that may look like a leiomyoma. These fibroids, especially the large ones, are important to document because they can affect the pregnancy once the baby starts growing. Leiomyomas may also look like a contraction. This is normal and go away after time. So if we see a possible fibroid and aren’t sure if it’s a contraction, continue with the exam and come back to the area to see if the enlarged structure has gone away. Using Doppler may assist in deciding between fibroid and contraction because fibroids usually present less vascular than a contraction.


Hi Amanda,
You are spot on with associating maternal age with pregnancy scans. This is a helpful tip. This is something I will take with me when I begin to scan OB's. You've picked a great differential. I'm sure it's very easy to mistake a contraction for a fibroid, thanks for the advice on going back on the exam to identify if it is in fact a fibroid or just a contraction.
Do you mind sharing the info on the vascularity between the fibroid and contraction? I'm interested to know how the contraction has more. I found this image on the fibroid, but didn't see one showing the contraction. I was trying to compare.
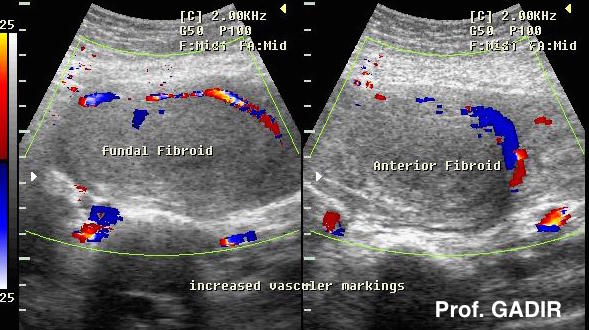
Hi Maria,
I got the information off of the lecture notes Michelle provided for us. I tried to Google some images of a contraction with color Doppler but failed to find any. I think a great explanation of why a fibroid has less vascularity than a contraction is because the uterus is flexing, causing a rush of blood flow to the area when contracting. While a fibroid still has feeder vessels, it doesn't need much blood flow than the constantly working uterus needs. I would think this would be more vascular than the picture you provided (and this is just a theory of mine).
I still think a better way to differentiate a fibroid and uterine contraction is coming back to the mass after completing the survey and seeing if it is still there or has gone away over time.
In my opinion, there are some abnormalities seen during first trimester ULS that are clearly abnormal. Ectopics, enlarged nuchal translucency, cystic hygromas, etc. are a few examples of exams that have a pretty clear sign that something is going on. However, as new sonographers, I feel like we will be more inclined to miss things that stray from normal in a subtle way. Especially because none of us seem to get very many first trimesters, our eyes are not going to be completely used to what "normal" looks like. These four images are examples of how sudden differences can be an early indication of future problems.
A)
B) 
C) 
D) 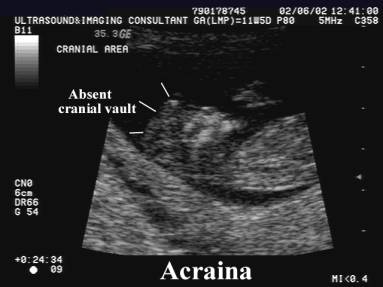
A) All these yolk sacs are slightly irregular. Irregularly shaped, too echogenic, too big, too small.
B) This gestational sac is too small for the normal sized fetus.
C) Separating gestational sacs from pseudosacs and knowing that we should not even suggest gestational sac without a secondary yolk sac visualized.
D) I'm not sure I would ever assume acrania. I think I would assume I was angled weird or the fetus was laying in a funky position.
All these are potentials to see in a first trimester. This is why it is so important to be diligent during these exams (along with all the other ones). If we can catch an irregularity early, it allows for better decision making opportunities.
Paris, I wish I could see more 1st trimesters, so far I saw only 2 and the sonographers performed them soo fast in like 5 mins! It seemed so simple, but now that we learn how many things could go wrong I know this exam is more then just gestational sac, yolk sac, ovaries and embryo. We really have to scan the mother anatomy carefully to not miss a big problem thats "growing" inside.
Great examples of the abnormal secondary yolk sac and gestational sac. I think as technology advances the first trimester scan will become more and more involved. As for now the most I've seen first trimester is a tiny embryo that I measured the CRL for. It had a heartbeat that we were also able to measure. The secondary yolk sac looked healthy as well. According to this website acrania can be visible around 11 weeks. https://radiopaedia.org/articles/acrania.It's super rare and to my eyes still a very vague image to recognize. Here's to hoping we all get a more first trimester experience soon!
Hi Paris,
I enjoyed looking at your images you posted. Very well put together. Seeing the different shapes and sizes of the yolk sacs in image (A) is a reminder that, just because we see one, doesn't mean its all good. We must evaluate the entirety of it. For image (B) What would cause the gestational sac not to grow as fast as the baby? and what happens if it never grows? Does the baby get smushed? I'm sadly confused. Image (C) you are 100% right, no secondary yolk sac, no gestational sac! And on image (D) i'm with you on that, I would keep tweaking the transducer, thinking it was operator error, but would never assume Acraina.
Hey Maria-
Here is the case study from image B. It is considered first trimester oligohydramnios. Some causes of oligohydramnios from last quarter include uteroplacental insufficiency, drugs, fetal abnormalities, or premature rupture of membranes. I'm not sure what the case was here, but these are some options.
To answer your questions - as you can see, if there is oligohydramnios early on, the fetus has a poor prognosis and will likely be a failed pregnancy.
Asymptomatic patient presented for first trimester dating study.




On this study 13 days later, the embryo has increased in size a little, but the contour is less well defined and there is no longer a heart rate.
On the first study, the difference between the mean sac diameter (14 mm) and the embryo crown rump length (12 mm) is less than 5 mm. Since the difference is less than 5 mm, this is considered "first trimester oligohydramnios" and is suspicious for a failed early pregnancy (although not definite).
On the follow up study 13 days later, there is no longer a heartbeat in the embryo. The early pregnancy has failed.
Hi Paris,
I know what you mean about assuming an acrania Dx. Acrania has several differential Dx to consider:
" Imaging differential considerations include conditions such as:
This is very true regarding success and failure in abnormalties in a first trimester scan being normal vs abnormal. For example The midgut herniation which is normal and will resolve by week 12 verses omphalocele which has a sac surrounding it or gastroschisis. Which doesn’t have a sac and Which will not resolve and is abnormal and should not appear during an OB survey.
Another success that could become a failure is success that the fetal brain is developing however the parts of the brain such as flax,choroid plexus,and hemispheres are all fused and not isolated. Holoprosencephally!
Holoprosencepally

Thank you, Jazmin for these images. No matter how many times I see omphaloceles alongside gastroschisis, it really helps to have the visual reinforced. At first glance, or if the image is obscured by maternal structures, it could be easy to mistake 1 for the other. It reminds me of the importance of being sure of dates and details going into an exam.
I think one of the topics we covered in class that is partial normal and not is the heterotopic pregnancy. They are rare hwoever may present in your time of scannin . Due to the fact a woman with this case is to have a IUP and a abnormal ectopic occuring at the same time! just like any other condition this one is crucial to identify in the first trimester to check the well being of the intrauterine pregnacy and identify the ectopic as soon as possible as it may rupture with time. I have yet to find if any screening test differ and can identify possibility of a heterotopic pregnancy. As of now I believe patients symptoms and background info is important to identifying possible heterotopic. Per radiopaedia, possible predisposing factors that can lead to a heterotopic pregancy are the following: hx use of a intrauterine contraceptive device, tubal surgery, history of PID and history of previous ectopic as well as ART.
I'd as well thought id list some differentials that may look similiary to a heterotopic pregnancy's that we are to consider in order to rule out other possibilites: a ectopic pregnancy with a intrauterine pseudogestational sac and a intrauterine gestation with a hemorrhagic corpus luteum
I'll be listing some images below today
Hello Liz,
Thank you for explaining heterotopic pregnancy so well!!! I struggled with this concept a little in quarter 3 I wanted to add a photo for those visual learners.
heterotopic photo: IUP/ECTOPIC SIMULTAEOUSLY
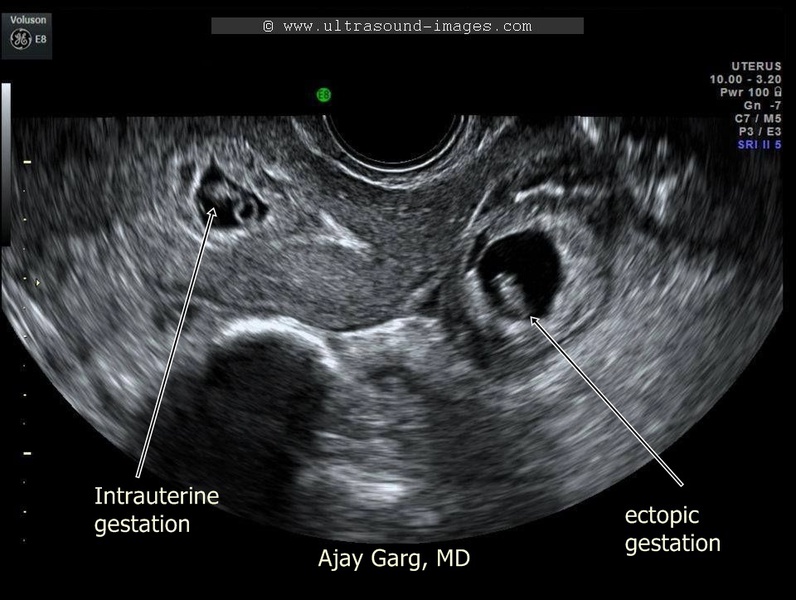
Hi Liz
I like the fact that you bring up heterotopic pregnancies because they do appear to be semi-normal with the one IUP. You may be scanning and see a normal intrauterine pregnancy with a yolk sac and gestational sac, but if you fail to thoroughly assess the adnexas, you could be missing an ectopic pregnancy, which we know to be a crucial diagnosis.
I think one of the biggest screening tests is simply hCG levels. I would think that hCG levels would be elevated, but according to sonoworld.com, “in a heterotopic pregnancy, only careful examination of the extrauterine anatomy provides the means of making the sonography diagnosis”. Although we cannot solely rely on the hCG levels to indicate a heterotopic pregnancy, we can use sonography along with this testing to determine if an adnexal mass is in fact another gestation.
hi Amanda! thanks for pointing that out! I thought a lab val would kinda gives us some sort of indication of possible heterotopic however I couldn't find anything other than thoroughly assessing your area via sono because anything could be lingering you just cant stop and stay content if your see a norm IUP you must further investigate
Hi Liz,
Thank you for clarifying heterotopic pregnancy. I wasn't really to sure the ins and outs of it when I first about learned about it, so i'm really glad you brought it up in our DB. According to the Journal of Human Reproductive Sciences, they explain, " The incidence was originally estimated on theoretical basis to be 1 in 30,000 pregnancies. However, more recent data indicate that the rate is higher due to assisted reproduction and is approximately 1 in 7000 overall and as high as 1 in 900 with ovulation induction." That is a 13,000 difference from past data to recent data. And saddening for women who's ovaries to do not mature fast enough, they get a treatment for ovulation induction, this increases their risk by even more of having heterotopic pregnancies.
With an Anembryonic pregnancy, the patient may be asymptomatic or have vaginal bleeding in early pregnancy. Due to the syncytiotrophoblast in the endometrium HCG is formed and there are clinical signs of a pregnancy including positive pregnancy test results. Unlike a normal pregnancy their hCG levels will fall over time. Sonographically there is a blastocyst but the fetal pole/embryo/secondary yolk sac will be absent. The uterus is decidualizing, but no double decidual reaction will be present. A secondary yolk sac means an actual pregnancy occurred.The mean sac diameter (MSD) will be ≥25 mm.
Normal DD reaction:

Anembryonic pregnancy:
This is a great distinction between the two - the decidual reaction, but empty sac and falling hCG versus the remaining yolk sac. There are so many factors to consider when examining such early potential pregnancies. There are a great many clues that present themselves to us just about the gestation sac - shape, size, contents.
Here is an informative recap of first trimester findings from the University of Massachusetts:
https://www.e-ultrasonography.org/upload/usg-19043.pdf
Hi Serina,
It is very important for a mother to have serial ultrasounds when experiencing a possible Anembryonic/Blighted ovum pregnancy. Remembering, that we can not a call a for sure pregnancy until we see the secondary yolk sac. hCG testing is also an extremely important screening to continue to follow up with, so we can determine if it is rising or falling. Great post! It really amazes me how the little things in the first rimester play a huge role for the pregnancy to be a success.
Would you be able to help answer this question, how many weeks until it is considered a missed pregnancy or in other words how long does the doctor wait for the yolk sac to appear?
Hi Maria, I have three sources here:
1. According to lecture:
12 mm gestational sac without yolk sac is a filed pregnancy.
2. According to radiopedia:
"...at 5.0 to 5.5 weeks, it can sometimes be seen as two parallel lines rather than a discrete circle. Yolk sac should be seen on transabdominal scanning when the mean sac diameter (MSD) is 20 mm or at a gestational age of 7 weeks and is usually seen endovaginally with an MSD of 8-10 mm or gestational age of 5.5 weeks."
Source: https://radiopaedia.org/articles/yolk-sac?lang=us
3. And this video form 123radiology says it should be seen at 5-5.5wks at 6:45mins in:
In the very first weeks of pregnancy, it is crucial to assess hCG levels with gestational sac size and maternal LMP. If a sonographer sees an empty gestation sac between weeks 4 and 5, but under the impression that gestation is farther along (5-7wks), it could very well seem like a failed pregnancy, whether complete AB or anembryonic/blighted ovum. In this situation, hCG and a correct MSD should clarify the finding.
4.7wk viable gestation sac
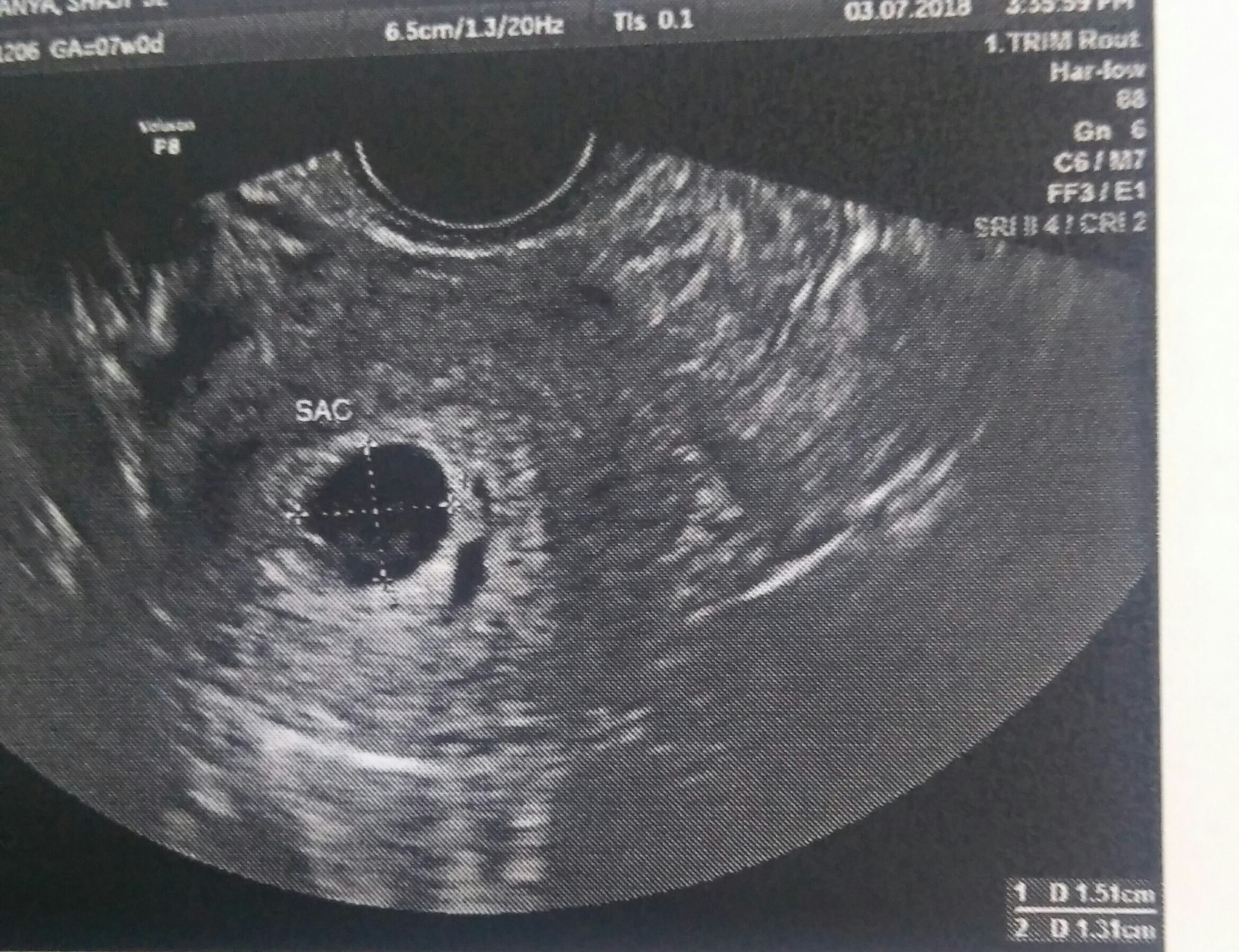
13mm empty gestation sac, most likely anembryonic.
Hey Beth,
LMP is so important when scanning a 1st trimester. I'm with Michelle, when she mentioned, she doesn't even want to start a scan on a patient without a hCG test, because then your really playing the guessing game. An empty gestational sac can mean a few things, miscarriage or possible be miscarrying, an ectopic pregnancy and of course the anembryonic pregnancy. Correlating the MSD and the hCG is the most important, thank you for sharing!
While my post in not necessarily a presentation, it is important in that it can be easily confused in the first trimester. Nuchal translucency (space between the skin that is behind the neck) is very important in that it is considered a soft marker of more generalized abnormalities. According to Radiopaedia a thickened nuchal translucency can be associated with aneuploidies such as: trisomy 21, and 18, and Turner Syndrome, and structural defects and syndromes such as: congenital diaphragmatic herniation, congenital heart disease, omphalocele, skeletal dysplasias, and more.
Utilizing incorrect technique is where one may confuse normalcy with pathology. According to Radiopaedia the correct technique is as follows
Use of the correct technique is essential:
This is a correct nuchal translucency

Abnormal nuchal translucency
In this photo you could see how one could mistakenly measure the wrong structure leading to further testing and anxiety in the parents

Hi Perresha,
During the first trimester, sonographers can see the subcutaneous fluid in the posterior region of the neck of embryos and fetuses. However, only large amount of fluid is associated with a higher risk of chromosomal and structural abnormalities.
Nuchal translucency (NT) is a very important screening test done by ultrasound in the first trimester of pregnancy – from 11 weeks to 13 weeks 6 days of gestation. After 14 weeks of gestation, most of the fluid is usually reabsorbed and the test has no diagnostic value.
To get reliable results, the CRL of the fetus should be from 45 mm to 84 mm. It is very essential that this test is performed by a certified in nuchal translucency sonographer; otherwise, the results cannot be used. Screening by NT can detect about 80% of fetuses with trisomy 21 and other major aneuploides for a low false positive rate of 5%. The combined detection rate of 90% can be reached if first trimester screening tests, such as NT, free β-hCG and PAPP-A, are used together.
It is helpful to know that when the nuchal translucency is <2 mm, the rate of aneuploidy is less than 1% (Knipe). Usually NT < 3mm is considered as a low risk. If we got >3 mm, the differential diagnosis will be an incorrect technique, as very clearly explained by Perresha. In addition, it can be fetal neck skin thickening due to first-trimester hydrops fetalis. Knowing the results of T1 screening tests will assist us in planning and adjusting our scanning protocols to find structural anomalies usually associated with aneuploides.
Reference: Knipe, H. Nuchal tranclusency. Retrieved from https://radiopaedia.org/articles/nuchal-translucency-1
Hi Perresha,
Your post was so great. Thank you for showing us the techniques involved with Nuchal Translucency. The two tiny parallel echogenic lines are so helpful identifying whats abnormal. It's helpful that the image only involves that fetal head and upper thorax so we can better asses the overall Nuchal Translucency. The image you showed with the mistaken Nuchal Translucency was hard for me to differentiate. Do you happen to know how many exams one needs to take to become certified to be able to asses the Nuchal Translucency?
To summarize this week’s discussion on first trimester success and failures we have learned that the first trimester is a very important time for an embryo to grow. They must be able to transition through the embryonic cycle with no complications, however given some circumstances not all embryos will make it. Here is a list of the success vs failures that we’ve came up with this week;
- Subchorionic hemorrhage vs Acute placenta hematoma vs Twin gestation
- Gestational sac vs Pseudo sac vs Blighted Ovum/Anembryonic vs Cyst
-Normal midgut herniation vs abdominal wall defects
-Rhombencephalon vs CNS abnormalities
-Cystic hygroma vs Cephalocele (frontal, parietal, orbital, nasal, and nasopharyngeal regions)
-Corpus luteum cyst ring of fire vs Ectopic pregnancy ring of fire
-Contraction vs Fibroid
-IUP vs heterotopic pregnancy
-Normal Nuchal Translucency vs Abnormal Nuchal Translucency
We all have agreed the dating is the most important factor to determine the age of the gestation, so obtaining the LMP from each patient will help. We also know that hCG screening test is essential in determining if there is a possibility of pregnancy. Serial hCG test may be considered to follow up if we see any discrepancies between the image and the levels of the hCG. This discussion board has helped me with differentials that I was having trouble understanding, thank you everyone for your help in making this week’s DB a success. Below I have attached some links for your review with some of the findings for 1st trimester success and failures.
https://radiopaedia.org/articles/subchorionic-haemorrhage-2?lang=us
https://www.sciencedirect.com/topics/medicine-and-dentistry/gestational-sac
https://onlinelibrary.wiley.com/doi/pdf/10.7863/jum.1989.8.5.255
https://sonoworld.com/Fetus/page.aspx?id=1096
https://radiopaedia.org/articles/pregnancy-of-unknown-location?lang=us