Why is it important to correlate the clinical history, presenting symptoms, and screening tests with sonographic findings, particularly in the first trimester......in other words-what becomes red flags for us when we start painting the diagnostic picture and why?
Discussion Board Week 2.............
It is pertinent to have HCG labs to determine what you are visualizing during your scan. If the levels are high, pt is bleeding or experiencing pain and has a positive pregnancy test you want to evaluate the uterus for a gestational sac and yolk sac or fetal pole. If there nothing visualized, evaluate the adnexa / ovary region to ensure there is no risk for a suspected ectopic pregnancy. If there is no gestational sac, no ectopic pregnancy, it could be an early IUP.
If there is something located on the adnexal area and a gestational sac is residing in that region, another alternate could be that it is just a large corpus luteum cyst, but it should be evaluated. Using Color Doppler can help one differentiate. If there is no yolk sac inside, it's hard to tell. It should display low impedence, however it's similar flow to an ectopic pregnancy. It can get dicey.
Lastly having an understanding of what possible differentials can be if AFP levels or low or high. If they are low, potential chromosomal abnormalities such as Trisomy 18,13, 21. AFP levels high can indicate twin pregnancy. The spectrum is large on differentials. It will take one to be thorough with checking patient history, labs, and not rushing through your exams to ensure your diligence.
Hey Charissa! Critical thinking question!
Let's say you have a pt that has hCG levels that are elevated and the order says "r/o ectopic."
You start your exam TA and your patient is completely gassed out. Her bladder is not filled and you are struggling to see anything.
You start an EV ULS and there is no sign of an ectopic, however, you can't see either ovary.
Do you let the patient go? What would you do in a situation like this knowing an ectopic pregnancy is very dangerous for your pt.?
If this were my patient, I would perform both exams as normal noting decreased ability to visualize due to overlying bowel gas and lack of appropriate window. I would not send the study to be read by the radiologist and would instead message them that the patient is coming back at XXX time. I would give the patient bottled water and ask her to drink the entire bottle while I watched. While she is drinking the water I would tell her not to use the bathroom and explain the importance of the test and obtaining quality images because what the doctor has ordered can quickly become life or death. I would then put her back in the waiting room. I would continue with my schedule and finish my next patient; then I would call her back in (regardless of my next patient and how backed up I would become) and try the exam again (under the same order). By this time there should be a better sonographic window and hopefully less bowel gas to obtain quality images. However, if she does leave before I come back to her, then at least I have tried and can rest knowing that I did all that I could do in my power.
Hi Paris! I would use color doppler on the adnexa region to see if I can obtain anything. I would use pulse wave and evaluate the spectral waveform to see if any low resistive flow was coming through. I would also ask a colleague to take a look as well. Lastly, I would give her water and have her walk around and attempt again after my next pt to give her time to fill her bladder. If I still was not able to view it, the provider may recommend another modality like an MRI. What would you do?
Perresha and Charissa-
You guys seem to think pretty similar. I assume our thoughts will differ based of situations we have seen at our sites. I guess if I had time to have the patient drink water and walk around I would try that first. I would try to avoid having the patient leave and then come back in after the following patient because I think that would cause them to worry. Honestly, I think I would call the radiologist or the ordering physician and ask how they would like me to navigate the situation. Especially if I was seeing signs/symptoms of an ectopic, I would be hesitant allowing the patient to leave.
I also like the idea of having a coworker coming in for a second look. Sometimes a fresh set of eyes is all it takes.
Thanks for your input ladies!
Hey Everyone! Welcome back! This is a topic I personally need more practice with. So often I get a work order and just quickly get to work. I look up their history to see if they have had any relevant ultrasounds or CT's, but if they haven't then I just start with my exam. However, just as we discussed in class, lab work and screening tests are crucial for determining the course of the exam. For instance, without looking at blood work, I wouldn't necessarily know to look for an ectopic pregnancy. As we saw today in class, an early gestational sac can easily mimic a corpus luteum cyst. Without having looked into her hCG levels, we wouldn't know to document anything that may look suspicious or even just cystic. In addition, I have found that sometimes what it says on a patients work order is not the whole story. Talking with a patient about the symptoms they have been experiencing, medical history/surgeries, and family history can really impact how you do your detective work. For instance, a patient might be coming in for pelvic pain/pressure. As I'm scanning she may tell me about a palpable mass on her left lower side. If I can palpate it, the red flag comes out and I am immediately going to focus more closely on her adnexa. In a profession where it's already easy to miss things, having the most information we can get allows us the ability to avoid a miss.
What are three of the most important questions you think you should ask a patient during a first trimester scan? Also, if you had it your way, what labs would you want every patient to have done before they came in for a first trimester ultrasound or R/O ectopic?
Most important questions:
- LMP for gestation age
- Procedural history (i.e. cesarean, oopherectomy, cervical cerclage, etc)
- Parity, gravidity, number of abortions
Labs everyone should take:
- RH + or - test to find out if the mother needs to get a RhoGam shot. If a mother is RH - then she will need the shot, so she will not develop antibodies against a RH+ baby. This is very important to development and survival of a pregnancy. So this test should always be taken no matter if the mother is visiting ultrasound or not.
- hCG or beta- hCG levels should always be identified before going to ultrasound. Otherwise a sonographer and radiologist will not be able to differentiate normal vs. abnormal findings.
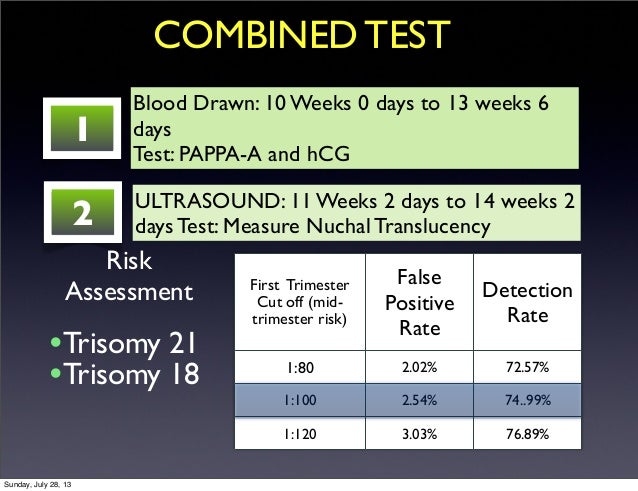
- Now we combine the first trimester screen to include nuchal translucency, hCG, and PAPP-A. All of these are helpful when imaging ultrasound because results of the screens guide the exam. Normal results will make the exam more routine. While abnormal results can put the pregnancy on a better management plan and more time can be allotted for exams that are expected to be more detailed.
- Nuchal translucency and PAPP-A help more for the 2nd and 3rd trimester exams.
- hCG is helpful in the first trimester because we can correlate expected size with the patient's given LMP. We can also discern if we should be seeing IUP or not. If hCG is nonexistent we can rule out ectopic. If hcG is double the normal amount that correlates with our imaged gestational sac size then there could be a possible ectopic pregnancy. Without hcG level tests exams would have less direction and could easily miss an abnormality.
Hey Jackie! I love how thorough this answer is.
All those questions are crucial to ask the patient and most of them are even required. However, I love that you recognize how important previous abortions are for our studies. Sometimes this can be a sensitive area of discussion, however, I like to think of myself as an advocate for the patient. Getting all the information that could potentially guide their exam is going to be beneficial for them in the long run.
How do you think you could convey this to a patient to help them feel comfortable enough to talk about past abortions?
Usually, I don't ask out right. I ask about number of pregnancies and number of births. Then I ask about cesarean and past surgeries or procedures. If they there is a difference in pregnancies and births then surgical history will help with deducing if there were purposeful or spontaneous abortions. Although admittedly I did have a case with a patient who had 4 pregnancies. She was in her high 70's with no surgical history. And she told me she was pregnant 4 times but only had 2 children. As I was scanning her she was very talkative and asked me many questions. She began to talk about her personal life the more I exchanged with her. At that point I didn't mind all the talking, because her movement was minimal. I had assumed she had only given birth twice. But eventually she voluntarily told me that one of her children had died as an adult and one of her children was stillborn. So she only had 2 children left. In actuality she had 4 pregnancies and given birth 4 times. I changed it on the worksheet. That situation ended up being a good lesson in making sure to get clear answers. It was my fault. I hadn't asked the right question. Instead of, "How many children?" it should be "How many time have you given birth?" That is a more accurate question for the information we need.
At my site we don't usually fill out the "AB" box on the begin page. We don't normally do OB unless it is an urgent or emergency exam.
While the above example worked out for me to get the necessary information, in the future I would say to not be shy when asking about abortions. It is a medical procedure or medical occurrence in the case of spontaneous abortions. And we are not here to judge, so the patient shouldn't feel judged when we are asking them about it. The number is just a stated fact and will help in her future care.
Psychologically, having an induced abortion is a choice. And having a spontaneous abortion happens. If the patient is in the office, then they are willingly seeking advice. So they would be willing to divulge the information we ask of them as long as we are professional and honest in our actions to assist them.
Here is a website talking about the psychological affects an abortion might have on a woman. While we may not be affected by a patient's abortions, we should be sensitive to their emotions. We can educate ourselves by reading this:
Do you require psychological counseling after you have had an abortion?
Headings in the article include:
How do women feel after an abortion?
Every woman is unique in how she feels after an abortion. Most women report feeling a sense of relief that they have made the best decision under the circumstances. This is the most common response. For some women, however, abortion can raise a number of emotional responses including sadness, guilt, rage, shame and regret. Some women feel bad about themselves because they don’t feel guilty about having an abortion, but think they should feel guilty. In general, understanding your emotional pain can help you to begin to let go of the grief, guilt, rage or shame you may be feeling. It is important to acknowledge that you are hurting and to take good care of yourself if you are experiencing difficulty.
You are not a bad person because you had an abortion. You are also not alone in having chosen abortion. Many women are surprised to learn that about 42 million women worldwide have abortions each year.
What kinds of things might contribute to a woman feeling distress after an abortion?
Is it normal to feel depressed after an abortion?
What is “Post-abortion Syndrome"?
What can I do to help myself heal after an abortion?
Hello Jackie!
I completely agree with your 3 numbered important questions and answer to obtain prior to staring an exam as I myself have similar ones like so on my post! As for your screening test I have a neat chart I found online for visual sake, breaks it up as to what test is performed on specific time of pregnancy. HCG is a very reliable tool, it is to be used to correlate with your findings and as well provide a better study

Hi Paris!
I agree, as mentioned in our critical thinking class- Investigate, making our hypothesis, analyzing labs / priors, gathering any other additional info from the pt and lastly evaluating will always promote a better outcome. Three important questions I would ask aside from Name and DOB; LMP, how many children including miscarriages / abortions, and if they have any medical history that includes diabetes, pre-eclampsia, etc. I would request HCG labs, otherwise I'm going in blind.
Although these questions may seem personal and off putting they are extremely helpful as a sonogapher to give us clues as to what we can expect during a first trimester scan. First we need to know LMP, history of any pregnancy (full term, abortions (spontanious or otherwise) still births, infertility, etc), it's also important to know about any prior surgeries. Prior surgeries can be from C-section, oophorectomy, D&C, all of these can impact a future pregnancy and the appearance of the uterus/adnexas.
For an early first trimester a current hcg is ciritical as well as any prior values for comparison. Below is from Kaiser on what labs are expected for their first prenatal appointment. There aren't many labs listed that would be helpful for ultrasound findings. Results from the nuchal translucency screening would be helpful for a later first trimester appointment. Results from PAPP-A would also be helpful in knowing if the embryo had a higher risk for Down syndrome or other chromosomal abnormalities.
Heather I love this, thank you! It seems pretty disappointing that I had to read this at the end...
"Coverage for prenatal tests and exams varies by health plan. Certain tests, even if recommended, may not be covered depending on your health plan."
It's unfortunate that there may not be equal opportunity for parents to be as prepared as possible for the journey they are about to embark on.
If you had a friend that was pregnant, but didn't have health insurance, which tests would you recommend as being more important? Any more than others?
That would depend on my friends risk factors. Lets assume my friend is young and healthy like I was when I had my kids with no family history. I would say the basic first trimester blood draws and ultrasound would be sufficient. No need for the PAPP-A or amniocentesis when the risk factors are low. However, if those tests came back abnormal I would encourage the next level of testing. Even with extra cost it would be worth the benefit of knowing what challenges lie ahead if the pregnancy is continued, like any additional medical care the baby or mom may need.
We get a lot of patients in the ED who don't have a primary care for their pregnancy. The come in with having no prenatal exams or care. I would say the most important after hCG to confirm pregnancy is the RhoGam/ Rh test. I think if there is pathology and a patient doesn't get treatment then the pregnancy will run its course whether that be to full term or as an SAB or still birth. The RhoGam shot is an easy fix compared to aneuploidy which is indicated by the other screens. If I could only do one, I would do that one. The rest is up to the dice.
Of course an ultrasound paired with hcG is planned for these patients. If you considered ultrasound to be a screen. Then I pick that one.
Talking to our patients is one of the best things we can do to gain the most information. I would start by asking the LMP, followed by if the patient has had any surgeries, such as C-sections, removal of the ovary, hysterectomy, etc. I would definitely ask if the patient has ever been pregnant (abortions, miscarriages, deliveries, etc.). I honestly wouldn't stop there. I've been scanning patient's who have been coming in bleeding and having pain that it makes me want to get to the bottom of it. I in fact talk to them throughout their whole time and learn as much as I can so I can correlate the findings.
I would indeed want every single patient to have a hCG test. This can tell a great deal of information as we scan the patient.
Great answer Maria! I feel the same way. The more information, the merrier. One of the first questions I ask after the required ones is, "How has your pregnancy been going so far?"
This is the time they usually say things like, "I've been really sick, I've been having some spotting, cramping, etc., or things have been smooth sailing." Asking about their experience is a great way to build a strong rapport which can ease their mind when having to ask about past abortions and the more difficult questions.
Now that you have been doing OB's a bit, do you think you will start with just the mom in the room or will you bring people back automatically? As we mentioned in class, sometimes these patients have some secrets that they are not ready to share with the person in the room.
Hi paris,
I think I would still want just the patient in the room. I would rather not have all eyes on me while scanning, it makes me nervous. Who knows, once I become efficient enough I may allow it. Unfortunately we still don't get to scan outpatient OB's, but we do get ER patient's who come in for rule out for ectopic and other complications with pain and bleeding while pregnant in the first trimester. We've had a few torsions while pregnant, that was interesting.
Hey Maria,
I feel similar. However, I think once I have scanned through the baby and made sure everything looked okay, I would be happy to bring in their loved ones. I know it's a special time and, if it were me, I wouldn't want anyone excluded from that special appointment. But I agree that starting without anyone but the scheduled patient is best to ensure you are getting all the necessary questions answered promptly and honestly.
Thanks girl!
Hi Paris,
Here are three questions I find helpful to ask during a first trimester scan:
How many pregnancies have you had? Very helpful in determining gravida and parity of the mother, which also starts a further conversation about how those went and if any complications had occurred.
Have you had any surgeries in your pelvic region? This is important to know because, as we learned on Monday, a C-section scar is a possible location for implantation to occur, causing an ectopic pregnancy.
Have you had any symptoms, pain, bleeding, etc? Some patients may experience bleeding and may mistake this as being a normal symptom of pregnancy due to this being their first time becoming pregnant or just a lack of knowledge.
I would love for the Econsult to have hCG levels listed right under patient's LMP or EDD. I would have an idea of what to look for before even putting the transducer down.
Very efficient Amanda!
From there if there are any red flags, I'm sure you would do some further investigating with your questions. You're so personable and I bet your patients will feel very comfortable giving you any information you need :)
It sounds like you have a great plan of attack for these exams!
What's an E-consult?
Do you look in the patient's chart before the exam for previous lab results?
We look in the chart and can see them if they were done or if they were ordered an not done yet.
Econsult is the order with the patient's name, exam type, indication, and OB's will have the patient's due date on there as well. I was saying it would be nice for the hCG levels to be listed their as well, or maybe only be listed if they came back abnormally high or low. This way we would could quickly see this information before grabbing the patient and beginning the exam, and yes if we look at the patient's labs we would be able to see it there too.
I agree about the hCG levels, Amanda. This is like the fist step. I also like to ask how they are feeling this morning, this usually makes them feel this process is fully about them and patients really open up and relax for every exam :)
Hello Paris,
The three most important questions I would ask a first trimester patient would be:
Have you ever been pregnant? why because I feel this question is a direct yet, open ended question. For example, if I was to ask how many children do they have? they could include children they didn't birth for instance if they have a stepchild or foster child. Next i would ask is have you ever had any miscarriages/abortions? specifying so hopefully I can get information on AB, ectopics, etc. Another question would be do you remember your last menstrual period, I feel asking in the first trimester can help you determine what you should be seeing; a yolk sac, fetus, or even the heartbeat.
Most importantly the lab values to get all my patients checked would be blood type against the babies to make sure her body won't produce antibodies against it. Next, I would want all patients to have a pregnancy test, AFP, HCG, & STD test.
Good call on the STD test! If that isn't already in their records, it is SUPER important that her medical team is aware so we can best support her.
Liz posted a really helpful chart showing the different labs that are done during first trimester. If you're at all unclear about what tests happen when, make sure you take a look! It really cleared things up for me and helped me organize the order.
Also, great questions! I can tell you're interested in providing the best patient care!
I didn't even think of STD testing. Is that included in the first or second semester screening? I remember them running those tests for me, but I can't remember at what point in the timeline it was done. I do remember seeing all the numbers and risk "chances" for Maximo having down syndrome, etc. All they say is negative for STD. I should look it up in my online medical profile. I bet it's in test results somewhere.
Thank you Paris, I also was thinking of a drug test. We had a patient that was on drugs not sure how the baby made it to 20weeks for a OB survey but the baby was really small and the mother was sleep the entire time. It was in her chart that she had a history of drug use based off her appearance and slurred vocabulary I am sure she was on something so sad.
Hey Jazmin,
While I agree that having the mom on drugs is TERRIBLE for her baby, it's also the patient's decision to due so. Her medical team wouldn't necessarily be able to use that information to enforce a certain lifestyle. I'm not sure if it would help us substantially on our exams because if wouldn't change our responsibility. We can be as thorough as possible and if something is wrong, more lab work (like drugs) could help a physician understand why things are going wrong.
I like where your mind is at though! If only everyone wanted to create the best and healthiest environment for their baby to thrive.
Hi Paris,
I would like every one of my patients (pregnant women) to have first trimester screening tests done, including nuchal translucency, hGC, PAPP A and fcDNA. First trimester screening integrated test has a higher detection rate (90%) than NT (60-75%) and biochemical markers (65%) alone, or even second trimester screening tests, such as triple test (70%) and quad test (76%). In addition, collecting personal and family history is crucial. We cannot assume anything by just looking at a patient, we need to know facts. I like my classmates responses on collecting personal history. I just would like to add that I might ask my patients if there are any diseases that are running in their families, such as polycystic kidney disease, heart anomalies that I should be aware of. In addition, it will help me to plan my study if a pregnant woman can disclose information if her children have congenital defects or structural abnormalities.
Why is it important to correlate the clinical history, presenting symptoms, and screening tests with sonographic findings, particularly in the first trimester......in other words-what becomes red flags for us when we start painting the diagnostic picture and why?
The first example I can think of is when imaging a C-section scar ectopic pregnancy.
Red flags:
- high hCG level but no IUP (Question: but isn't the LUS part of the uterus? They must call it ectopic just because it is not in the body of the uterus. Can it implant only in the myometrium? or go through the scar and implant on abdominal muscle? In that case would it be abdominal ectopic)
- gestational sac located in the anterior lower uterine segment instead of the body of the uterus
- thin layer between the bladder and gestational sac
- misshaped gestational sac that is more thin or linear due to the location of implantation inside the scar
- heavy bleeding
The following I found from https://ectopic.org.uk/professionals/caesarian-scar-ectopic-pregnancies/
The evidence suggests that these pregnancies, if they continue, will be associated with the placenta becoming deeply implanted into the scar and often through the scar into the space between the uterus and the bladder. If the pregnancy survives, the placenta then fails to come away at delivery and there is a very high risk of severe bleeding, needing a hysterectomy to control bleeding or worse. Early in the pregnancy these scar pregnancies may also bleed heavily.
~~~~~~~~~~
It is important to correlate the clinical history of the maternal patient having a previous c-section. Without that knowledge the reasoning for the location of the gestational sac is not as apparent and it may be harder to diagnose. Also presenting symptoms for heavy bleeding could be do to the deep infiltration of the placenta near or closer to the cervix. This is similar to ectopic cervix symptoms. A high hCG or continou rise of hCG can help to diagnose an ectopic and differentiate the c-section scar ectopic from an aborting pregnancy because of the LUS location. Instead of it being on the way out we can evaluate the labs and use doppler to rule out an AB vs. a still viable ectopic pregnancy.
Hey Jackie,
Great question about the LUS. It seems like it is part of the uterus so it should be fine for a blastocyst to implant in this area. However, as I'm hoping you can see from this image, it is dangerously close to the cervix. Think about how much baby grows and how this could be a predisposition for placenta previa, cervical funneling, and other problems. Also, from what I am seeing, it's becoming more common to see LUS ectopics because that is also where cesarean scars are located.
Therefore, the most ideal implantation site is the superior and posterior wall of the uterine cavity. I hope this helps!
Sonographically, some structures during pregnancy look very similar or are indistinguishable from others and, without lab values, may be described or diagnosed incorrectly. hCG values are important to tell us whether the gestation process is under way or how far it might be along. hCG is also correlated with measurement of the gestation sac - because these increase proportionately, a discrepancy could lead a sonographer to image structures more closely. If hCG is elevated, but an IUP is not seen, a sonographer would closely check ovaries, cervix, etc for an ectopic pregnancy. A grossly elevated hCG, as correleated with gestational sac size and LMP, could indicate a molar pregnancy, which brings me to another important piece of the puzzle - obtaining the mother's LMP in order to check against both the hCG and gestation sac size. Additionally, it is important to ask about maternal procedures, scars, gravida/para/abortus, possible trauma, maternal medical treatment secondary to pregnancy (medications, etc). There are many points in an OB scan where a sonographer questions what they see; knowing the patient history can enable us to make important distinctions in both our investigation and our report. Without knowing these pertinent details, it would be possible to mistake an ovarian ectopic for a dominant follicle, which could be life threatening.
This article on RadioGraphics lays out thorough information regarding normal and abnormal first pregnancy findings regarding my above mentioned correlations:
https://pubs.rsna.org/doi/10.1148/rg.2015150092
Hey Beth! Thank you for the very detailed response! If you had a first trimester OB come in they had all the necessary lab work completed, which abnormal test would give you the biggest red flag? What levels would that test be at?
I feel that there isn't just 1 example that is the biggest red flag. There are a few cases: 1) if the hCG had previously been appropriately elevated and afterward showed a decline (various AB), 2) hCG is elevated beyond what is indicated by gestation sac size/LMP, but there is only 1 embryo (possible heterotopic), 3) hCG approx 2000 with no gestation sac (ectopic), and 4) hCG is grossly elevated (approx 10x) the most likely is a variation of a molar pregnancy.
Yes Beth! I love how your mind is working here. You clearly recognize that you have to stay open minded because each case is different! Things can change in an instant and elevated hCG shouldn't make you assume the worst. However, it should make you very diligent in your scan. There are many things you are trying to rule out, but it doesn't mean you should go in panicked. All we can do is document our findings and write a story.
Thanks for your thoughts!
Combining the clinical history, presenting symptoms, and screening tests with sonography will give us an idea of what to look for. If for instance a patients is coming in from the ER is in her late 30's with pelvic pain and bleeding, had prior tubal ligation and positive pregancy test I am automatically going to be looking for an ectopic pregnancy. If I didn't have her medical history I could mistake an pseudogestational sac for an early IUP and miss a life threatening condition. Similarly if there was no lab work to go off of and I knew the patient had tubal ligation, I may not be looking for an ectopic pregancy. It is vital to get in the habit of asking questions and looking up lab values. It's something I'm still learning how to do and I'm thankful for my clinical instructors who share their insights and instincts with me.
Heather, today I was told that OB's and breast exams are the two patients sue most over. I think it's a good idea to prepare the patient for all the questions so they know they have to answer in detail and not feel they should withhold some info from us because when asking we seemed to be in a rush or their family is making them uncomfortable. I agree it takes time to build these good habits because when I first came in I was just happy to get scan time.
Elona,
You're right. Maria and I were discussing that it seems like a safe practice to bring the patient in by herself first. This can help ensure that a patient is more comfortable asking honestly.
I remember when I used to have my mom come into doctor's visits with me. At some point, doctors used to ask my mom to wait for a moment before they allowed her to come in. They would ask me questions such as, "Are you sexually active, do you drink/smoke, do you feel safe at home, etc." My doctor always ensured me that she wasn't going to rely anything we discussed to my mom. It made me feel more comfortable answer uncomfortable/difficult questions.
I believe we should have that same standard to offer the best patient care possible. And I think while at first they may feel frustrated, they will begin to appreciate it when they realize it's in their best interest. Do you agree?
Hi Heather,
I like your critical thinking. If a patient had tubal ligation in the past and now her hCG is elevated, we need to rule out an ectopic pregnancy or even heterotopic pregnancy if IUP present. We always need to keep in mind that tubal ligations, salpingitis, PID could change the normal tubal function and ability to move a zygote toward the uterus; therefore, it will stuck in the fallopian tube and try to implant there.
It is important to correlate the clinical history, presenting symptoms, and screening tests with sonographic findings because all together can point to a couple or a specific disease/anomaly. In the example of an ectopic pregnancy a patient can present with a triad of bleeding, adnexal mass, pain, and a history of previous ectopic pregnancies. These three together plus a positive HCG and her history will most likely tell us that the woman probably has an ectopic pregnancy, especially if it is known that she has had other ectopic pregnancies before. Another patient comes in at the age of 18 with signs of extremely elevated HCG levels, vaginal bleeding, and hypertension then we would think that maybe it is a molar pregnancy. We know it couldn’t be an abortion because of the extremely high levels of HCG, age range, and a high blood pressure.
It is important to correlate clinical history, presenting symptoms, and screening tests with our findings in a first trimester ultrasound because it can give us a sense of direction before we put down the probe. I think of it as a movie review before going to see the actual movie. Clinical history should include gravida (times becoming pregnant) and parity (giving birth). I usually gather this information by asking mom, “So is this baby number 1, 2, 15?” and that not only gets mom talking but also makes her think I’m hilarious. One question that I find difficult to ask is if mom has had any abortions or miscarriages, so if anyone has a way to bring that up without worrying mom about the current pregnancy I would greatly appreciate it!
Presenting symptoms are important because they aid us in looking for pathologies, such as cramping associated with subchorionic hemorrhage or nausea/vomiting associated with ectopic pregnancies. Patients may think these are normal symptoms of pregnancy and fail to tell us what symptoms they’re having. This is why it is important we ask the patient these questions. With screening tests, I specifically think of hCG. These levels are extremely important because it can indicate a potential problem with the pregnancy if the levels are too high/low. For example, when scanning and you visualize an IUP, you might think that it appears to be a normal pregnancy. But, if you were to look at the hCG levels and see that they are elevated based on patient's LMP, you should carefully evaluate the adnexas for a possible heterotopic pregnancy.
Hey Amanda!
I agree, talking abortions can really put some patients in an uncomfortable situation. An easy way to do this is to talk about the kids they have at home. If she is G2 (this pregnancy being her second) P1, try asking about the child she already has. This will be a very smooth opportunity for her to tell you if that child is no longer around, how the pregnancy was with that child and so much more. It's just important to gently and compassionately navigate these conversations.
You mentioned symptoms being an indication for guiding your exam. I'm wondering, what symptoms might a patient be experiencing that would turn on your red flag alert?
Hi Paris,
A patient experiencing vaginal bleeding would turn on my red flag alert. According to the book and lecture from Monday, the most common occurrence of bleeding in the first trimester is from subchorionic hemorrhage. But this symptom can indicate a wide range of other possible pathologies, such as an absent intrauterine sac or placental hematomas.
Hey Amanda!
Before Monday, vaginal bleeding during pregnancy would sound the alarms for me too! However, after we talked more about it, I'm now under the impression that some light bleeding or spotting, especially during the first trimester, is very common and often nothing to be concerned about. However, a heavier flow would still concern me.
Are we on the same page with this or am I missing something?
Hey P,
I believe we are on the same page. Vaginal bleeding is common in the first trimester, and what I found in the book was that the most common Cause of this bleeding is subchorionic hemorrhage. Yes, a heavier flow would definitely be more of a concern, and depending of what I see when scanning I would start to think some type of abortion has occurred if, for example, the fetus is nowhere to be seen but products of conception are still visible.
Hey Amanda,
I'm glad we're on the same page! I remember we said in class that 50% of pregnancies bleed and 25% of them go on to be fine. I guess you're right though. Those numbers are not comforting enough for me to say, "Oh she's just experiencing some bleeding, no biggie." I would definitely make me roll up my sleeves and start searching for the reason behind the bleed.
Thanks for working that out with me!
Correlating the history, symptoms and screening test is literally to help put the pieces of the puzzle together. Without the given information, we cannot have a steady foundation. One thing that stood out to me during the lecture, was how excited these women are feeling to think they are pregnant. Early symptoms of a normal pregnancy and ectopic pregnancy can be very similar; missed period, tender breast, and maybe some nausea. An hCG test may even be elevated. A red flag during the 1st trimester can be bleeding and pain in the abdomen, this can mean that instead of a normal pregnancy there is a chance of an ectopic or a threatened abortion.
I found this flow chart online, It was helpful to me to see the next steps during first trimeter complications.

Maria I am LIVING for this chart. This is the perfect way to show at how many points things can quickly take a turn. It's also a nice way to show that even though a problem occurs, it doesn't always mean something detrimental.
Thanks for the share!
In the field that we are entering, being able to correlate clinical history with presenting symptoms and screening tests to the sonographic findings is all in the name...Diagnostic Imaging. Without pulling all of these aspects together and presenting our case with the pictures as proof it would be very difficult for the MD reading the images to create a report. Their ability to create the report is based on our ability to obtain images that correlate symptoms, history, and screening tests.
I think that the most important test is the beta hCG. Is it at a level where we should be able to detect a pregnancy sonographically? Is it doubling appropriately, or beginning to decline? Is it way too high for where she is at in the pregnancy? All of these questions leads to different paths in the picture I am trying to create in my mind. It is also important to get accurate information concerning symptoms they are currently feeling, have subsided, or may not seem relevant to them. Symptoms can help guide in the physical direction or location where one may want to take extra care or a closer look. It is important to pull all the information together for the best possible outcomes.
Exactly! We are diagnostic medical sonographers and without making these connections we would just be photographers. I like to think we are prettyyyy much doctors because correlating hCG levels and gathering information from the patient's chart is not always enough information for us, especially with first trimester exams. Asking the patient about any symptoms gives us so much more knowledge and also reminds the patient that we are there to provide the best care possible for her and future baby!
Hello Perresha,
Yes, we want the best possible outcomes for our patient. I am learning that first trimester can be tough the embryo is at such a vulnerable stage and literally getting sick and taking over the counter drugs to feel better could harm the embryo. With mostly half of women experiencing some bleeding during the first trimester, leaves it up to us as diagnostic sonographers to determine if the bleeding is caused by a normal trophoblastic reaction from the implantation of the embryo or is the bleeding from a spontaneous abortion. Those were just a few examples of normal and abnormal reasons for bleeding. However, during the first trimester there is so much that could possibly be going on and it is up to us to narrow it down to normal or abnormal and then determine a cause and effect. I totally understand when you mentioned in your post that questions lead to different paths. Nice to have this as a discussion topic so we could all get an idea of which test are going to be important in the first trimester because of the rapid formation of the fetus.
PC I love the way you said this! Poetic almost. You're right. It's so important that we know what we're looking at and that we know what normal should look like. If things are looking funky, it's our responsibility to provide as many diagnostic images to show the radiologist what is going funky. This is why knowing the embryology and the normal growth rate is crucial.
Having the hCG is ideal, however, if a patient hasn't had any lab work, we should still be able to do our job. Document all that we see!
Thank you for your thoughts!
I believe it is highly important to correlate the clinical history, presenting symptoms, and screening test for the first trimester to in a sense expect or get an idea as of what your possibly going to face. Its best to prepare with such valuable info as all these help you as a in all aspects as of going with the I.M.A.G.E concept sonographer correlate your findings with your valuable info. It's essential for you as a sonographer to use all these tools starting from basics such as collecting info from patient pertained to the G,T,P,A,L , gathering your patients LMP, perhaps your patient is AMA ( advanced maternal age), and screening test ofcourse as well as knowing your dating parameters for normals. 1 trimester eval includes sono evidence of the : gestational sac,yolk sac(we see 2nd) fetal pole and heart. As for a red flag I'm going to use an example, my answers as from the book as a reference. Patient comes ( not sure of LMP) positive HCG levels normal UT however no gestational sac seen via US. what could possible be outcomes? i have 3 please correct me if i am wrong. 1. very early IUP 2. non developing pregnancy 3. possible ectopic. This goes to prove how important that HCG test is, gives you the green light to further analyze other possible outcomes seen no 1st tri sono structures seen.
hi Liz, I like how you use I.M.A.G.E. to help you come to a conclusion of what could be wrong with the patient. It is important to note the First day of their last menstrual period, previous pregnancy’s, abortions, miscarriages, cesareans, and if they are taking any hormones. I think you are correct on what can possibly be happening with the patient.
Hey Liz,
I love this question. My thoughts-
I'm not sure if number 1 is an option. You mentioned that the UT was normal. However, if a patient has positive HCG that would mean that a blastocyst has already implanted and we would at the very least be seeing a noticeably thickened endometrium. Also, without knowing the HCG level specifically or the LMP, it's difficult to say if it's a possible ectopic or a non developing pregnancy because I would think either way the UT would look somewhat enlarged or there would be some sort of FF for an ectopic. Again, evey situation is different and it would depend on how far along she was. It may require her coming back.
Thoughts?
Hey Paris!
sorry I wasn't clear, I meant normal UT for pregnancy with the endo of course thickened however no gestational sac seen. I did question number one as our HCG levels are indicating pregnancy as we should be able to distinguish something via sono however I got that from our hagen ansert book. I still have yet to see a case as such in real to put two and two together. All those are probable possibilities from our book I agree with two and three however I do question number one as well. thanks for the feedback!
Great use of your sonographic reasoning! In early first trimester only a few blood draws are routinely done, and then you may also have the NT results if its later in the pregnancy. If your patient is advanced maternal age she may have access to further screening early. Being of advanced maternal age is more common and comes with additional risk factors for mother and baby. A test that is often recommened is the cell free DNA test. This additional testing is also beneficial for my second trimester anatomy scans too. The parents often already know the gender and risks so they come in much more relaxed and I'm able to focus on scanning instead of fielding nonstop questions. I did have an excited dad try to snap some pictures on his phone today. I felt bad when I asked him to stop per HIPAA, but assured him I would send some printed pictures home.
RED FLAGS
Lets start with the basics: (bullet points are "red flags")
- Patient comes in with the classic triad of pain, bleeding, and as you are scanning you notice an adnexal mass and no fluid in the endometrium.... Ectopic pregnancy.
- Patient comes in with the classic triad of pain, bleeding, and as you are scanning you notice an adnexal mass and fluid in the endometrium......The first thing is to check the fluid in the endometrium. I would be looking for the double decidual reaction, and I would also be looking for the secondary yolk sac. This will help me determine if it is a pseudo sac or gestational sac.
- Patient comes in with multiple bilateral cyst seen within adnexa, nausea, pain, with grape like vesicles seen in the uterus......Theca lutein cyst caused by a molar pregnancy.
- Patient comes in with cervical dilation, heavy bleeding, no passage of embryo but no heart rate of embryo detected, with cramping & pain,......inevitable AB
During lecture I recall the Alpha-fetal protein levels will be high if the fetus has anencephaly because the brain will be in the amniotic fluid causing the levels to rise. I also recall if the HCG levels are over 2000 you should see a embryo. Correlating the history and lab results before beginning your scan will help and determine your protocol. Even if its simple, for example we had a patient with one fetus however she had products of conception and debris adjacent to the placenta my CI was spending so much time on the area and the patient asked her can you see the twin that didn't make it. It was clearly in her chart that she had begun with twins via IVF but we were running behind and didn't check. So take the time to check the priors sono sistas!
I feel like the priors literally save my life at times...just being able to look at what the uterus looks like, its lie, and sonographic appearance is a game changer. For me, in my mind I already know what "normal" looks like (if the prior was "normal") so I am somewhat cheating but it makes me more aware of what "abnormal" for that patient would look like.
Love the layout of your post Jazmin! So thoughtful.
I also wanted to add that if a patient had a molar pregnancy, her HCG levels would be abnormally high. That could be another sign to look out for.
Thanks for your helpful post!
YES! checking that chart is so important, but an easy thing to overlook when the schedule is booked up. A rise in AFP could also indicate multiple gestations. The patient you used as an example probably had high AFP's while the twin was still alive. I wish I had more experience with first trimesters, but I have only scanned them a few times and it was either too early to see anything definetively or it was a miscarriage. The poor mom with the miscarriage was so distraught. What other tests/values do you think would be helpful for evaluating an early first trimester pregnancy?
Hello Heather,
Other test would be a blood test to check the HCG , and pregnancy associated plasma protein (PAPP-A). A STD test because some STD are non curable such as HIV & genital herpes and other STD can be cured but, its time sensitive and maybe the mother does not know she is infected and it could pass to baby. Also, a Nuchal translucency would be helpful to detect early fetal abnormalities especially if the mother is over 40yrs old.
I love the way you have organized your bullet points, Jazmin! The simplicity and logic really illuminates these presentations -> possible issues and really creates a handy set of tools. And I additionally agree about checking priors - it's one thing if the patient has no priors, but going in blind seems dangerous, especially on patients who have complex hx or recurring issues.
Hello Jazmin,
thanks for including the case scenarios and indicating what our next step would be. That's right I remembered AFP levels were noted on lecture but I couldnt quite remember. Thus AFP is elevated may indicate a probable anencephaly due to brain matter free floating in the amn fluid. I agree if HCG levels are at 2000 you should be able to see an embryo another indication you should be able to visualize an embryo is if the gestational sac is msd 25mm just another tip for ya!
One good example of why correlating clinical hx, symptoms, and screening tests, with sonographic findings during the first trimester is important is regarding Molar pregnancies. Molar Pregnancy aka Gestational Trophoblastic Disease, is more likely to occur in women younger than 20 and women older than 40. They will experience symptoms such as Nausea and Hypertension. In terms of labs they will have Increased HCG at 10 times the amount for the same age of a normal gestation. This remains elevated after 60 days. Sonographically their ovaries will have Theca Lutein cysts which will appear as grape like vesicles. A complete molar will have chorionic villi without fetal parts, yet still have a trophoblast which appears as grape like clusters. This form of the condition is related to choriocarcinoma whereas a partial form of the condition is not.
All this talk about screen tests and how they correlate to expected findings got me thinking about all the tests I got when I was pregnant. I wondered about how easy it would be to look them up on my health profile. I took the liberty of finding all of the tests done on me when I was pregnant. So here's an over share!
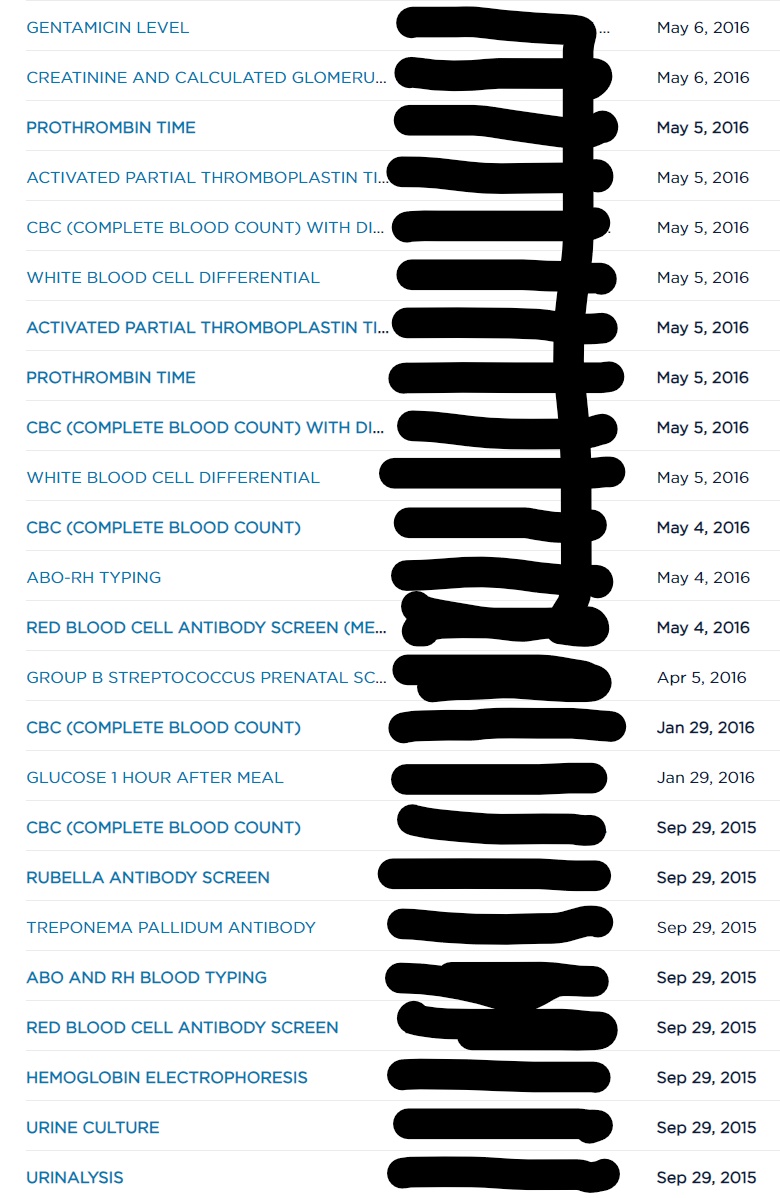
It wasn't as easy as I had thought it was going to be. First off, all the tests weren't in the test results tab! Some of the pregnancy tests were only shown as ordered in each individual office visit. So, I could have missed some, because I didn't click and look through all of my OB office visits..just the mile stone ones. I had to google some of these tests. I only bring it up because Liz had brought up STD testing during pregnancy screening. From the list and Google I learned that Treponema is a syphilis screen. You can see they also tested me for Strep and Rubella. Maximo was born on May 4, 2016. But I included the tests after that, because I stayed in the hospital due to infection from possible my c-section or my catheter. I just learned that they ran a Gentamicin test on me. That's an antibiotic test. And they did creatinine and calculated glomerulus test on me? Kidneys? I wonder if that is part of regular postpartum care or just me. I was in the hospital an extra 5 days.
But at the beginning they ran all the tests we've been talking about: hCG, PAPPA-A, ABO- RH.
They also did a urinalysis every single time I went into the office..probably to get my hCG levels.
They kept checking my blood cell levels. I wonder if that's to make sure I'm getting enough nutrients, oxygen, and making enough blood cells... Have to feed the baby! Diffusion!
Before even scanning a pregnant woman, we need to gather clinical history, screening tests results, ask the woman about presenting symptoms, personal history of using IVF, the number of abortions, miscarriages and living children, as well family history of chromosomal anomalies to get an idea what might be going on and on what we should focus on. Red flags for us can be following:
- Abnormal 1st trimester screening test results, such as nuchal translucency more than 5 mm (Hagen-Ansert, 2018, p. 1306), low hCG and PAPP A suggests chromosomal anomalies, such as Down Syndrome. So we plan our exam accordingly. We might see duodenal atresia, absence of the nasal bone, and echogenic bowel. The size of the embryo or fetus will be much smaller than expected dates. IUGR usually diagnosed with Trisomy 21.
- Extremely high level of hCG, hyperemesis, uterus size more than dates by manual examination might suggest molar pregnancy (hidatitiform mole ). Therefore, we might expect to see hydropic villi filling the uterus and theca lutein cyst in ovaries, depending on the type of the gestational trophoblastic disease.
- An IVF patient came in for a first trimester ultrasound and happily told us that 6 embryos were transferred and her hCG levels are skyrocketing now. Our train of thought might be: “Is it a high risk pregnancy? Will we see two, three or even six embryos in the uterus? Is there a heterotopic or pregnancy? Can we see hyperstimulated ovaries with a lot of cystic structures?
- A pregnant woman came in with the hCG levels lower than the gestational age (8 week) with a history of an ectopic pregnancy 5 months ago. She had bleeding, pelvic pain and a palpable adnexal mass. As we already know, a previous ectopic pregnancy is the strongest risk factor for developing an ectopic pregnancy again. The possibility of a repeat ectopic pregnancy increases significantly (threefold) with the number of prior ectopic pregnancies. It is very important to differentiate because an ectopic pregnancy is still a leading cause of maternal death in the first trimester of pregnancy in the United Stated (mortality rate 9-14%). Can it be an ectopic pregnancy in this case? Yes, it can because the chance of ectopic pregnancy is high in this case. Clinical symptoms, lab results and patient history could be a red flag to explore adnexa very carefully. Even if we found an IUP, it is a good idea to look closely at adnexa anyway because it can be heterotopic pregnancy as well.
Ellen I like that you brought up the heterotopic pregnancies that I forgot to mention in my post. Just finding a normal pregnancy is not enough to think we've completed our job with the gestational sac imaging, we have to evaluate the rest of the pelvis carefully because if a woman is not in pain and shows no reason for concern this ectopic will show itself later.
Hey Ellen,
Great reminder about asking for family history such as chromosomal anomalies. I'd like to add that this is something that should be asked BEFORE we start scanning. Once I was scanning and realized I forgot to ask the patients. I casually asked if they had any family history of chromosomal anomalies or problems with pregnancies. My patient immediately looked worried and said, "no why??" I think she thought that I was seeing something that sparked that question.
The purpose of these questions is to let the patient know that they are in thorough and quality hands, not for them to feel worried!
Thanks for the share!
It is is necessary to gather as much relevant information as we can before the exam in the first or second trimester. Its important to know priors before the patient comes in and once they do its good to have them share a little bit of info about how they’ve been feeling and what’s been happening lately. Not all information can be accessed in their charts and the doctor’s orders can also sometimes be ordered with mistakes because they clicked some wrong button. This is why I find it so much more relaxing to have the family wait for a little bit so that we can ask questions about pregnancies, how the patient is feeling so they can relax and really be themselves. When there’s family in the room this serious exam turns into a party where in many situations relatives just want to see the pipi and talk about how they were guessing what the baby was. It is much better with couples from what I’ve seen because they’re more patient and care about the purpose of this exam.
The first trimester scan can tell us a lot from the beginning just from the ultrasound. The foundation of our exam is the hCG levels that tell us a patient is undergoing changes. The measurements of the gestational sac can be correlated with the dates. If we see a normal gestational sac in the uterus that is growing according to the dates it makes the job easier and the next step is to evaluate the rest of the pelvis carefully- look at the adnexal areas, ovaries make sure there are no masses, calcifications, cysts and free fluid. If we are not seeing a gestational sac at 5 weeks in the correct place with high hCG levels this is a start to a long investigation to a pregnancy with uncertain viability.
One of the scariest complications that stood out to me and may be very common are ectopic pregnancies. They are increasing due to contraceptive devices, infertility treatments and surgeries. The nasty part is that they tend to repeat in patients that already had them. This is why it is so good to ask questions before the exam starts when no one is there and she will not want to avoid talking about these unpleasant memories. Asking this during the exam will definitely alarm the patient and they will be angry and worried that something is probably not well with their pregnancy. A positive pregnancy test, no intrauterine sac are already enough for concern and if a patient is bleeding or in pain and there a mass seen on ultrasound are good signs of a possible ectopic. Ectopics seem scary to me as a new sonographer because it can cause death and it is hard to distinguish from a mass with a cyst. It is pretty rare to find an ectopic in adnexa that will have a visible fetal pole. This is just another reminder to take time to sweep very well for every exam.
Im really hoping to see more 1st trimesters where there is soo much focus on mother’s anatomy vs a second and third where most attention is on growing baby.
Hey Elona,
You're right, there is a lot of information that we can gather and even diagnose from a first trimester ultrasound. However, there was one pathology in particular that we discussed in class that we should not actually diagnose until the second trimester because it is possible that a false-positive diagnosis can be made at gestational ages of less than 18 weeks. This is possible because the development of the cerebellar vermis is incomplete.
Do you remember which one this is?
Hey guys!
What a great discussion this week! It seems like we are all feeling pretty comfortable recognizing normal vs. abnormal (didacticly anyway). It's pretty clear that checking the hCG levels, (along with other labs) is what many of us find crucial in guiding us through possible differentials. It's also clear that many of us see the significance of asking our patients pertinent questions such as LMP, G and P, family history, symptoms they're experiencing, and others. It seems like an elevated hCG level, vaginal bleeding, and pain are three components that are sparking everyone's red flag alerts. This is awesome! As we know, each patient is different and the outcomes can vary, but it should definitely light a little fire under our booties to be super super diligent in our scans.
Thank you everyone for participating so much this week! I'm so glad to see we are starting the quarter off strong! This is A LOT of information to retain and we are really going to need to work together and practice it repeatedly to help us remember! Great work Sono Sistas!